A groundbreaking study by researchers at Harvard T.H. Chan School of Public Health, in collaboration with international colleagues, has successfully mapped all the genes essential for blood infections in Plasmodium knowlesi (P. knowlesi), a malaria-causing parasite in humans. This comprehensive genetic map is the most complete classification of essential genes in any Plasmodium species to date and holds significant potential for identifying new drug targets and understanding mechanisms of drug resistance.
The study, set to be published on February 6, 2025, in Science, highlights the urgent need for novel malaria treatments as drug resistance continues to threaten existing antimalarial therapies. “We hope that our findings are a major step for the field of malaria research and control,” said co-corresponding author Manoj Duraisingh, John LaPorte Given Professor of Immunology and Infectious Diseases. “Emerging drug resistance to the small number of antimalarial drugs is a growing problem. This map will be an invaluable resource to help researchers combat one of the leading causes of infectious disease death around the world.”
A Major Step in Malaria Research
Malaria remains a significant global health challenge, with approximately 249 million cases reported annually, leading to about 608,000 deaths. Among the various Plasmodium species responsible for human malaria, P. knowlesi is an emerging zoonotic threat, particularly in Southeast Asia, where its lethal potential is becoming a growing public health concern.
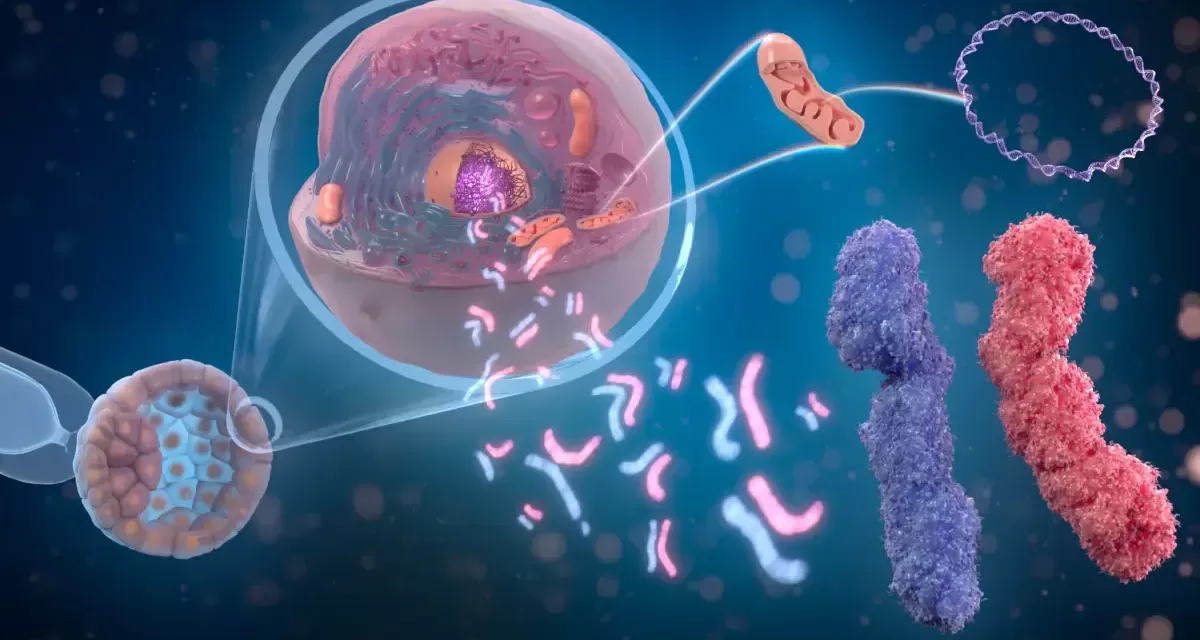
Using a cutting-edge genetic technique called transposon mutagenesis, the research team systematically disrupted non-essential genes in P. knowlesi, thereby identifying the full set of genes necessary for the parasite’s growth in human red blood cells. This large-scale genomic approach enabled the team to determine key molecular mechanisms that drive parasite survival and drug resistance.
“Knowing all of the essential genes in P. knowlesi allows us to understand the molecular strategies that the parasite takes to grow, to respond to environmental changes, and to respond to therapeutics such as antimalarials,” said co-first author Sheena Dass, postdoctoral fellow in the Department of Immunology and Infectious Diseases. “This molecular blueprint will help malaria researchers in the design and execution of biological studies of malaria as well as inform strategies to monitor and limit the emergence of drug resistance.”
Implications for Malaria Treatment and Drug Development
Beyond P. knowlesi, the research findings provide critical insights into P. vivax, another malaria-causing species that remains difficult to study due to its inability to be cultured or genetically modified in laboratory settings. Since P. knowlesi and P. vivax share evolutionary similarities, this new genetic map may aid in understanding P. vivax and developing more effective treatments against it.
The research team included Brendan Elsworth and Sida Ye as co-first authors, with Kourosh Zarringhalam from the University of Massachusetts, Boston, as a co-corresponding author. Other contributors from Harvard Chan included Jacob Tennessen, Basil Thommen, Aditya Paul, Usheer Kanjee, and Christof Gruring.
The study received financial support from the National Institutes of Health (grants 5R01AI168163, 5R01 AI167570, ORIP/OD P51OD011132, and U42 PDP11023), the Swiss National Science Foundation Postdoc Mobility (fellowships PBSKP3_140144 and P300P3_151146), and the Food and Drug Administration Intramural Research Program.
Disclaimer:
This article is for informational purposes only and does not constitute medical or scientific advice. Readers are encouraged to refer to the original published study in Science for more detailed information and to consult health professionals regarding malaria treatment and prevention strategies.