Oxford, UK – In a promising breakthrough, researchers at Oxford University have unveiled a new blood test, TriOx, which leverages the power of machine learning to detect multiple types of cancer at their earliest and most treatable stages. This innovative technology offers a potential game-changer in cancer diagnostics, particularly in the early detection of cancers that are notoriously hard to identify.
Published in Nature Communications, the study highlights how TriOx analyzes multiple features of DNA circulating in the blood, making it capable of detecting subtle signs of cancer. This could provide a quicker, more sensitive, and minimally invasive alternative to existing detection methods.
The test showed an impressive ability to identify cancer across six different types, including colorectal, esophageal, pancreatic, renal, ovarian, and breast cancers. TriOx not only detected these cancers but also accurately distinguished between individuals with and without cancer, offering hope for early diagnosis when the disease is most curable.
“Catch cancer early, and it’s more likely to be treatable, saving both lives and healthcare costs,” said Professor Anna Schuh, Professor of Molecular Diagnostics at Oxford’s Department of Oncology and lead researcher. “This blood test represents a significant advancement in early cancer detection, and while it’s still in development, it holds great promise for improving survival rates by making early diagnosis routine.”
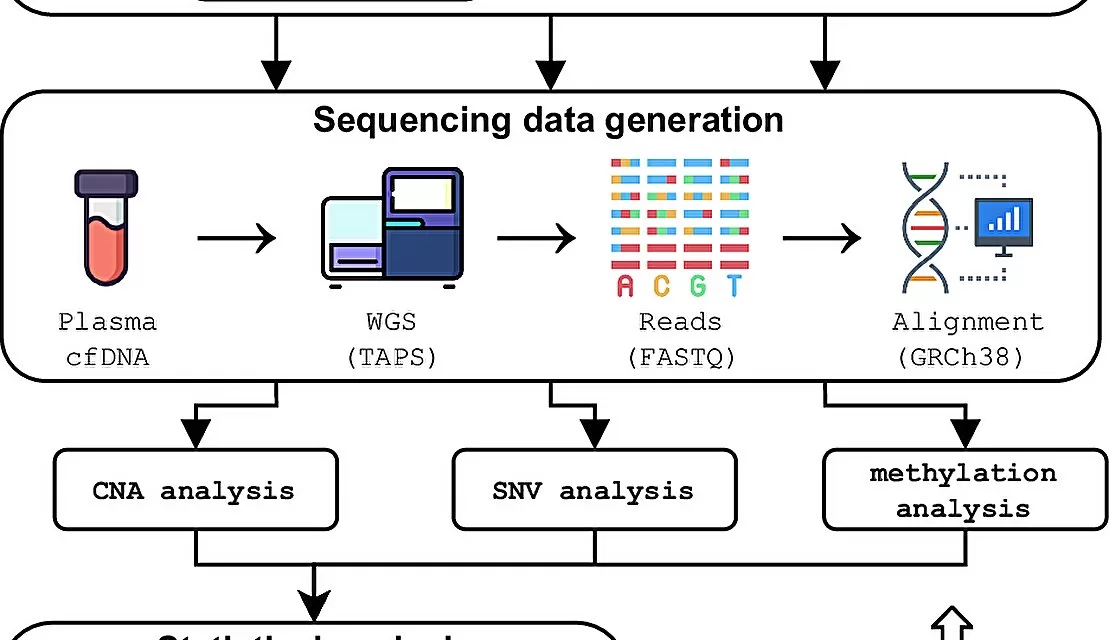
The TriOx test uses a combination of TAPS (Targeted Analysis of Plasma Sequencing), a cutting-edge DNA analysis technique, and machine learning algorithms. This approach significantly enhances the ability to detect small amounts of cancer DNA, making the test highly sensitive, even in early-stage cancer cases.
The test was evaluated using blood samples from both cancer patients and healthy individuals. The results were striking, with TriOx achieving a 94.9% sensitivity rate and 88.8% specificity. This means it can accurately identify cancer while minimizing the risk of false positives, ensuring patients without cancer are not subjected to unnecessary treatments.
Dr. Dimitris Vavoulis, co-lead researcher at Oxford’s Wellcome Centre for Human Genetics, emphasized the potential impact of the test, particularly for cancers like pancreatic and ovarian, which are often diagnosed too late for effective treatment. “Our approach could provide a simple, non-invasive solution that enables early detection of multiple cancers, which could ultimately save lives and reduce healthcare costs,” he said.
As the research team works to expand the test to detect even more cancer types and refine its accuracy, they are also investigating ways to integrate TriOx into routine healthcare, similar to cholesterol or blood sugar tests. The ultimate goal is to make early cancer detection as commonplace as these regular health checks.
While TriOx is still in its early stages, the promise it holds for transforming cancer screening and saving lives is undeniable. With further research and development, this breakthrough could become a cornerstone in the fight against cancer, offering a quicker, more accessible way to detect and treat cancer in its most treatable stages.
For more information:
Dimitrios V. Vavoulis et al, Multimodal cell-free DNA whole-genome TAPS is sensitive and reveals specific cancer signals, Nature Communications (2025). DOI: 10.1038/s41467-024-55428-y