The landscape of medicine has undergone a significant transformation over the last half-century. What was once a field rooted in expert opinions and anecdotal experiences has evolved into a highly scientific and data-driven discipline. From the introduction of evidence-based medicine to the advent of precision medicine, the way doctors make decisions is increasingly shaped by advanced technologies.
The Rise of Evidence-Based Medicine
In the 1970s, medical decision-making was largely based on expert opinion and clinical experience, with minimal empirical research to back it up. However, by the 1990s, the landscape began to shift. Researchers advocated for a new approach: integrating clinical expertise with the best available evidence. This led to the emergence of evidence-based medicine (EBM), a practice that prioritized high-quality research over anecdotal experiences.
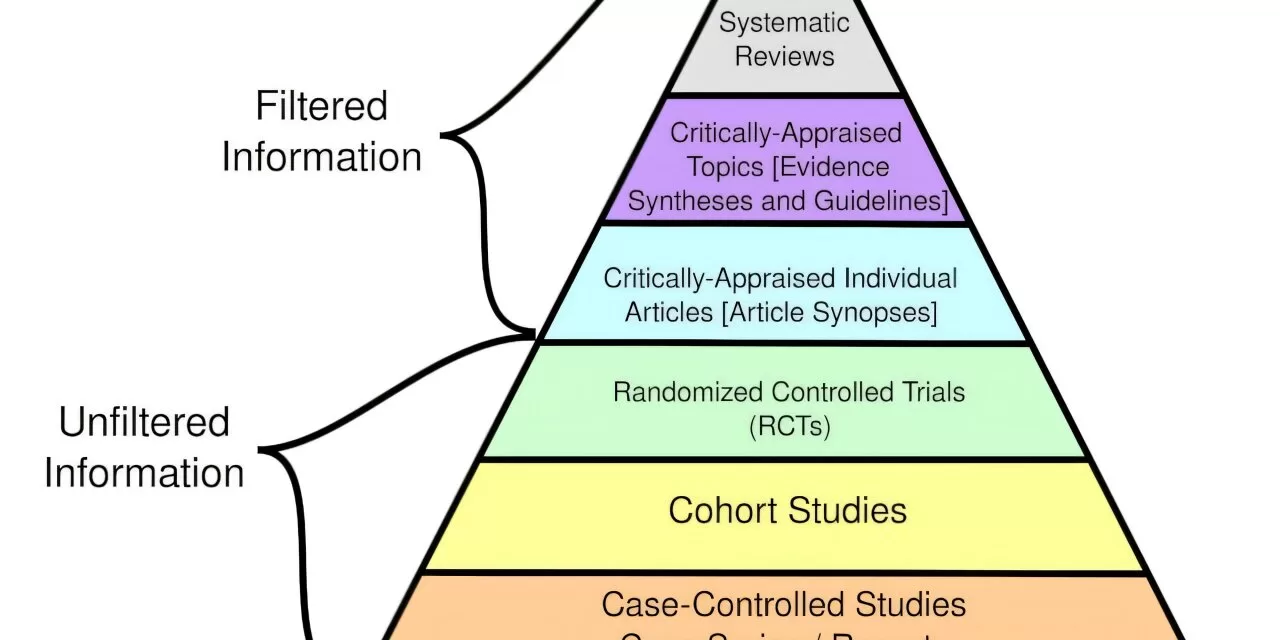
At the heart of EBM lies a hierarchy of evidence. Randomized controlled trials (RCTs), often referred to as clinical trials, became the gold standard. These studies allowed researchers to compare treatments in a controlled manner, minimizing bias. While observational studies and systematic reviews also played a role, they were seen as weaker compared to RCTs due to the absence of randomization.
This structured approach enables clinicians to ask specific questions about patient care, such as whether statins or lifestyle changes are more effective for lowering LDL cholesterol in a particular patient. By combining evidence, expert knowledge, and patient preferences, doctors can make more informed treatment decisions. Yet, the process of gathering and analyzing evidence can be time-consuming, which is why clinicians often rely on guidelines from established bodies like the World Health Organization or the National Institutes of Health.
The Dawn of Precision Medicine
While evidence-based medicine was gaining ground, two crucial scientific advancements set the stage for precision medicine. The Human Genome Project, completed in 2003, mapped the human DNA, helping scientists identify genetic variations linked to diseases and treatment responses. This breakthrough, combined with the rise of electronic medical records (EMRs), gave clinicians the tools to provide more personalized care based on individual genetic, environmental, and clinical factors.
Precision medicine allows doctors to tailor treatment to the unique genetic makeup and health history of each patient. This approach, however, brings new challenges. The sheer volume and complexity of data available today are overwhelming. How can clinicians determine which data is relevant for each patient? And how can they interpret this data effectively to make the best treatment decisions?
Harnessing AI for Better Medical Decisions
This is where artificial intelligence (AI) comes in. The growing complexity of medical data has made it impossible for doctors to rely solely on their own cognitive abilities. AI systems, developed by computer scientists in collaboration with geneticists, environmental scientists, and clinicians, are helping to address these challenges. By analyzing a wealth of genetic, environmental, and clinical data, AI tools assist doctors in making more accurate diagnoses and creating personalized treatment plans.
For example, AI can predict whether genetic testing is necessary for a patient based on their medical history and the likelihood of being prescribed medication influenced by genetic factors. Similarly, AI systems are being used to diagnose rare diseases by analyzing a patient’s genetic and clinical data, identifying patterns that may be overlooked by human clinicians.
The Future of Medical Decision-Making
The future of medical decision-making looks promising, thanks to continuous advancements in technology. Wearable devices that monitor physiological data in real time are already being integrated into patient care. These devices collect data on heart rate, blood pressure, and other metrics, which can be analyzed by AI systems to predict and diagnose diseases, ensuring more personalized treatment.
In precision oncology, for example, wearable ultrasound scanners are being developed to detect early signs of breast cancer, while skin-like sensors are being tested to monitor changes in tumor size. These technologies, combined with the ongoing expansion of genetic research and AI capabilities, will fundamentally reshape how clinicians make decisions and provide care over the next few decades.
As we move into this new era of healthcare, clinicians will continue to rely on evidence-based medicine, but increasingly, they will be empowered by AI tools and personalized data to make more precise and informed decisions. The future of medicine is a blend of human expertise, cutting-edge technology, and personalized care—ushering in an era where the patient’s unique genetic and environmental context is at the forefront of decision-making.