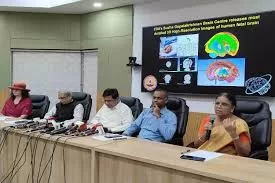
A groundbreaking advancement in tuberculosis (TB) diagnosis has been achieved by a collaborative team of researchers from the UK and US. The team, composed of scientists from the Rosalind Franklin Institute, the Universities of Oxford and Pittsburgh, and the National Institutes of Health, has developed a novel radiotracer for positron emission tomography (PET) scans, significantly enhancing the accuracy of TB detection.
This innovative radiotracer, named FDT, is designed to be absorbed by live TB bacteria within the body, allowing for precise identification of active disease sites in the lungs. Radiotracers are radioactive compounds that emit radiation detectable by PET scanners, enabling the creation of detailed 3D images. The development of FDT marks a significant milestone as it is the first time PET scans can be used to specifically locate active TB infections.
Following extensive pre-clinical trials with no observed adverse effects, FDT is now poised to enter Phase I trials in humans. The details of this research are published in the journal Nature Communications.
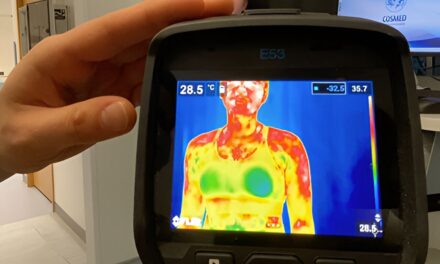
Current TB diagnostic methods include testing for the bacteria in a patient’s sputum and using PET scans with the common radiotracer FDG to detect lung inflammation. However, these methods have limitations. Sputum tests can yield negative results even when TB bacteria remain in the lungs, potentially leading to premature termination of treatment. Conversely, FDG-based PET scans can detect inflammation caused by conditions other than TB, and lingering inflammation post-treatment can result in unnecessarily prolonged medication.
The new FDT radiotracer overcomes these issues by targeting a carbohydrate unique to TB bacteria. This specificity ensures that the scan results accurately reflect the presence of active TB, thus improving diagnosis and treatment management.
A significant advantage of this new method is its compatibility with existing PET scanners and standard radiation control protocols, which are increasingly available worldwide. The production process for FDT is straightforward, utilizing enzymes developed by the research team to convert FDG into FDT. This simplicity allows for production without specialized expertise or facilities, making it feasible for use in low- and middle-income countries that bear the brunt of TB cases and fatalities.
In 2021 alone, 10.6 million people contracted TB, and 1.6 million succumbed to the disease, making it the second deadliest infectious disease globally, after COVID-19.
Professor Ben Davis, Science Director of the Franklin’s Next Generation Chemistry group, spearheaded the research. He emphasized the importance of accurately identifying active TB for both initial diagnosis and ensuring adequate treatment duration. “The common radiotracer FDG and the enzymes we’ve developed to turn it into FDT can all be sent by post. With a minimum of additional training, this effective diagnostic in essence could be rolled out into most health care systems around the world—and most importantly, in the places where this disease is still taking its greatest toll,” Davis stated.
Dr. Clifton Barry III from the National Institute of Allergy and Infectious Diseases highlighted the potential of FDT to revolutionize TB treatment and drug testing. “FDT will enable us to assess in real time whether the TB bacteria remains viable in patients who are receiving treatment, rather than having to wait to see whether or not they relapse with active disease. This means FDT could add significant value to clinical trials of new drugs, transforming the way they are tested for use in the clinic,” he said.
The new radiotracer FDT represents a significant leap forward in the fight against TB, offering hope for more accurate diagnosis, improved treatment monitoring, and ultimately, better outcomes for millions of patients worldwide.
More information: Distributable, metabolic PET reporting of tuberculosis, Nature Communications (2024). DOI: 10.1038/s41467-024-48691-6