New research has revealed the profound impact of sleep quality on a person’s immune system and its potential link to the development of chronic diseases such as obesity, diabetes, and cardiovascular conditions.
The study, published in The Journal of Immunology, found that even a single night of 24-hour sleep deprivation in young, lean, and healthy individuals altered the profile of immune cells, making them resemble those seen in individuals with obesity. Since obesity is known to drive chronic inflammation, this discovery highlights how the immune system is highly sensitive to sleep patterns and can rapidly adapt to changes. If these shifts persist, researchers warn they could contribute to long-term inflammatory states and increase the risk of disease.
The Link Between Sleep, Immunity, and Chronic Disease
There is already substantial evidence connecting sleep disorders and disturbances to chronic conditions like type 2 diabetes and cardiovascular diseases. While poor health outcomes are often linked to chronic inflammation, the direct influence of sleep on circulating immune cells—particularly monocytes—is less understood.
Monocytes are key players in the body’s innate immune response, helping detect pathogens and regulate inflammation. There are three types: classical, intermediate, and non-classical monocytes. Non-classical monocytes play a vital role in monitoring the body and responding to inflammatory cues.
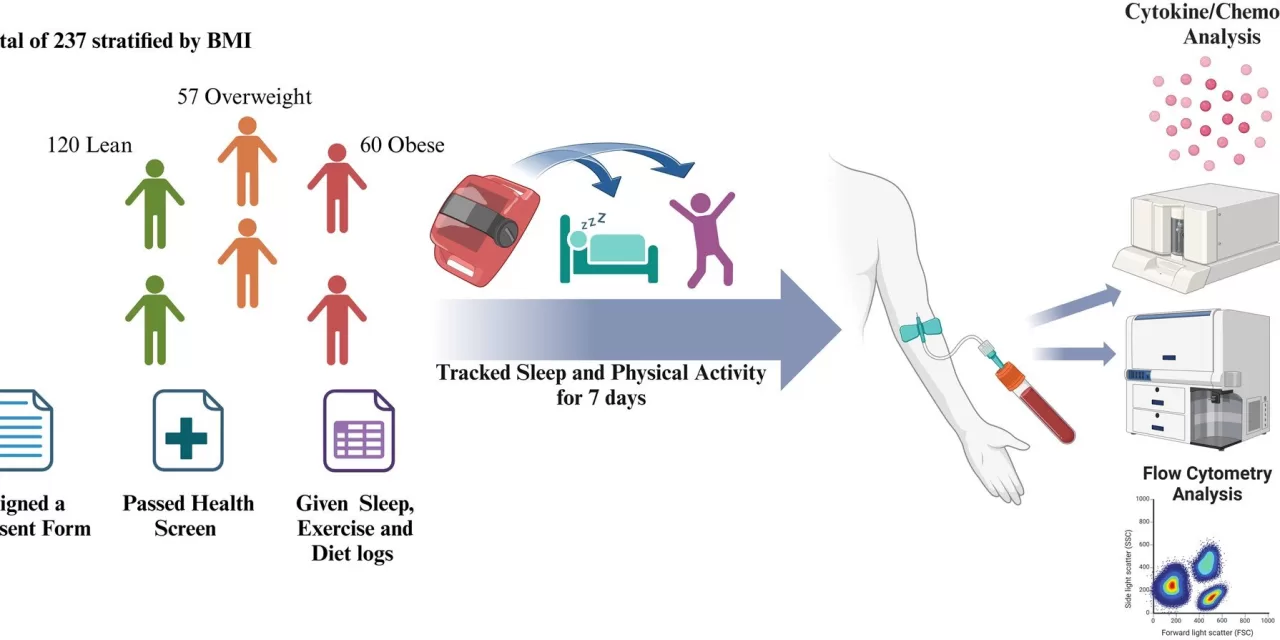
Researchers from the Dasman Diabetes Institute in Kuwait City analyzed the sleep patterns of 237 healthy adult participants with varying BMIs and collected blood samples to assess monocyte levels and inflammatory markers. Their findings indicated that obese individuals had significantly poorer sleep quality and higher chronic low-grade inflammation compared to those with lower BMIs. Additionally, they found an increase in non-classical monocytes in obese individuals, correlating with reduced sleep quality and elevated pro-inflammatory markers.
Sleep Deprivation and Immune Changes
To further examine sleep’s effects, five healthy, lean individuals participated in a 24-hour sleep deprivation study. Their blood samples showed changes in monocyte profiles similar to those observed in obese individuals. These findings reinforce the role of sleep health in immune function and inflammation regulation.
Dr. Fatema Al-Rashed, the study’s lead researcher, emphasized the growing public health concern, stating, “Advancements in technology, prolonged screen time, and shifting societal norms are increasingly disruptive to regular sleeping hours. This disruption in sleep has profound implications for immune health and overall well-being.”
Future Research and Public Health Implications
The researchers aim to further explore the biological mechanisms linking sleep deprivation to immune changes. They also plan to investigate whether interventions such as structured sleep therapies or technology-use guidelines can reverse these immune alterations.
“In the long term, we hope this research will inform public policies and strategies that recognize the critical role of sleep in public health,” Dr. Al-Rashed added. “By implementing workplace reforms and educational campaigns, we can promote better sleep practices, particularly for those most vulnerable to sleep disruption due to modern lifestyle demands. Ultimately, these efforts could help mitigate the burden of inflammatory diseases like obesity, diabetes, and cardiovascular diseases.”
Disclaimer
This article is based on recent scientific findings and is intended for informational purposes only. It does not constitute medical advice. Individuals experiencing sleep-related concerns should consult a healthcare professional for personalized guidance.