A groundbreaking study on the microbiome suggests that early-life exposure to certain gut microbes could play a crucial role in preventing diabetes, with promising implications for human health. The research, conducted on mice, revealed that the gut microbiota influences the development of insulin-producing cells in infancy, potentially reducing the risk of type 1 diabetes and even offering a way to restore metabolic function in adulthood.
The Critical Role of Early Microbe Exposure
Researchers discovered that mice exposed to broad-spectrum antibiotics in the early stages of life had significantly poorer metabolic health in adulthood. When the antibiotics were administered during a critical 10-day period shortly after birth, the mice developed fewer beta cells—insulin-producing cells that regulate blood sugar levels. These mice also experienced elevated blood sugar levels and reduced insulin production as adults.
“This, to me, was shocking and a bit scary,” said June Round, professor of pathology at the University of Utah Health and senior author of the study. “It showed how important the microbiota is during this very short early period of development.”
Through further experiments with different antibiotics, the researchers identified several specific microbes that positively affected insulin production and tissue growth. One particularly intriguing discovery was the role of Candida dubliniensis, a little-studied fungus commonly found in infants but not in healthy adult humans.
Candida dubliniensis and Its Potential to Prevent Type 1 Diabetes
The fungus Candida dubliniensis showed remarkable potential in protecting against type 1 diabetes. In genetically predisposed male mice, those exposed to the fungus during early life developed diabetes only 15% of the time, compared to 90% in mice that received a metabolically neutral microbe. This suggests that Candida dubliniensis could serve as a preventive agent for those at risk of developing type 1 diabetes.
Furthermore, exposure to the fungus seemed to promote the regeneration of insulin-producing cells in adult mice whose pancreas cells had been damaged. This is highly unusual, as beta cell regeneration in adults is not typically seen. The results offer hope for future therapeutic applications aimed at repairing pancreatic function in people with diabetes.
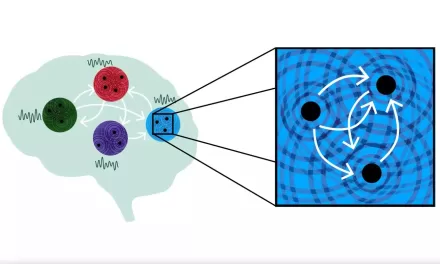
Immune System’s Role in Metabolic Health
The beneficial effects of Candida dubliniensis appear to stem from its interaction with the immune system. Previous research has shown that immune cells in the pancreas can support the growth of insulin-producing cells. In the current study, mice lacking a microbiome had fewer immune cells in the pancreas and poor metabolic function. However, when these mice were exposed to C. dubliniensis early in life, both their immune cells and metabolic function were restored to normal levels.
The study also found that Candida dubliniensis could only promote insulin cell growth in the presence of macrophages, a type of immune cell, highlighting the importance of the immune system in maintaining metabolic health.
The Future of Microbe-Based Diabetes Treatments
The discovery of Candida dubliniensis as a potential therapeutic agent raises hopes for new approaches to diabetes prevention and treatment. However, researchers caution that the beneficial effects observed in mice have not yet been proven in humans.
Jennifer Hill, the study’s first author and now an assistant professor at the University of Colorado Boulder, remains cautious but optimistic: “One possibility in the far future is that maybe signals like these could be harnessed not only as a preventative but also as a therapeutic to help later in life.”
Researchers also speculate that other, yet-to-be-identified microbes may offer similar benefits. The study marks an important step in understanding how early-life microbial exposure can shape long-term health outcomes, especially regarding metabolic diseases like diabetes.
A New Frontier in Diabetes Prevention
“Ultimately, I hope we’ll be able to identify these important microbes,” said Round. “By giving them to infants, we may be able to prevent type 1 diabetes altogether.”
While much remains to be learned, these findings offer a new frontier in the quest to understand how the microbiome can influence metabolic health and provide novel strategies for preventing and treating diabetes in the future.
Provided by University of Utah