When facing life-altering diagnoses, seriously ill patients and their families endure both physical and emotional turmoil. A single poorly chosen word or phrase from a healthcare provider can intensify this distress, eroding trust, diminishing patient agency, and complicating shared decision-making. Researchers, including Texas A&M University’s Dr. Leonard Berry, are emphasizing the importance of “compassionate communication” in medical care. In a recent paper published in Mayo Clinic Proceedings, Berry and his team highlight “never words”—phrases clinicians should avoid under any circumstance. Instead, they recommend approaches to foster empathetic, supportive language that empowers patients.
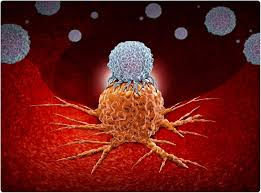
Dr. Berry, a Distinguished Professor at Texas A&M’s Mays Business School and a senior fellow at the Institute for Healthcare Improvement, explains that even as medical advancements continue, the “timeless” fears surrounding serious illness remain. “Patients facing advanced diseases, like cancer or end-stage heart and lung diseases, experience fear and complex emotions that can be compounded by the clinician’s words,” he says. Berry’s study, co-authored with experts from Detroit’s Henry Ford Health, asserts that language should ease, not add to, the emotional burden of serious illness.
Identifying Harmful Language: The ‘Never Words’ List
The researchers, drawing on surveys and clinical experience, compiled a list of phrases that can inadvertently frighten or disempower patients and families. These “never words” include statements like:
- “There is nothing else we can do.”
- “She will not get better.”
- “Withdrawing care.”
- “Circling the drain.”
- “Do you want us to do everything?”
- “You failed chemo.”
Berry points out that words like “fight” or “battle” may unintentionally place responsibility on patients to “win” against their illness, potentially making them feel as if they’re failing when health worsens. Instead, Berry recommends saying, “We will face this difficult disease together,” which underscores that patients have a team supporting them, no matter the outcome.
Language that Empowers and Comforts
To communicate more effectively, healthcare professionals can adopt alternative language that encourages open dialogue, acknowledges patient fears, and reframes potentially distressing statements. For instance, instead of the finality implied by “She will not get better,” doctors might say, “I’m worried she may not get better,” offering a softer expression of concern that leaves room for hope.
Berry explains that subtle shifts in phrasing can have a profound impact. Simple changes, like replacing “Do you have any questions?” with “What questions do you have for me?” invite patients and families to share their thoughts candidly, leading to better patient engagement and understanding.
Building Communication Skills in Medical Training
The study calls for incorporating compassionate communication skills into medical training. Berry notes that while medical education heavily emphasizes clinical skills, there is an urgent need to prioritize effective patient-centered communication. “Students and residents benefit from role models who demonstrate compassionate language,” he says. Mentorship is also crucial, as experienced doctors can share the lessons they’ve learned, showing younger clinicians how to recognize and replace phrases that might harm patient morale.
“Mentors can disclose phrases they have personally abandoned and show younger doctors how to adapt or correct language that doesn’t land well,” the study notes, underscoring the value of real-life examples in fostering a new generation of empathetic communicators.
A Call to Action for the Medical Community
By spreading awareness of “never words” and promoting a more thoughtful approach to language, the researchers hope to reduce unnecessary emotional suffering for patients and their families. They encourage medical schools and professional organizations to prioritize compassionate communication, aiming for a healthcare experience where words truly do no harm.
For further information, see: Rana Lee Adawi Awdish et al, “Never-Words: What Not to Say to Patients With Serious Illness,” Mayo Clinic Proceedings, 2024.