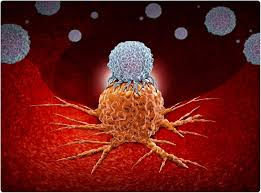
A groundbreaking study by researchers at University College London (UCL) and the Francis Crick Institute has uncovered a crucial link between immune cell disruption in the blood and cancer outcomes. The study, published in Nature Genetics, introduces a pioneering technique called Immune Lymphocyte Estimation from Nucleotide Sequencing (ImmuneLENS), which allows researchers to determine the proportion of key immune cells—T cells and B cells—using whole genome sequencing (WGS) data.
A Breakthrough in Cancer Research
The research analyzed over 90,000 WGS samples from the 100,000 Genomes Project, an initiative led by Genomics England and NHS England. Findings indicated that cancer patients have significantly lower levels of circulating T cells compared to healthy individuals. Moreover, a higher T cell proportion was associated with a 47% reduction in mortality over a five-year period following surgery.
Professor Nicholas McGranahan of the UCL Cancer Institute emphasized the importance of immune cell analysis beyond the tumor site. “Most immune system analysis until now has focused on the tumor itself. Our findings suggest that immune cells in the blood play a critical role in determining cancer survival,” he stated.
Clinical Implications and Future Research
The ability to assess immune system activity in the bloodstream could revolutionize cancer diagnostics and treatment planning. By incorporating ImmuneLENS findings into existing genetic diagnostic tests, clinicians could gain valuable insights into patient prognosis and personalize treatment strategies.
The study also noted that immune cell depletion occurs earlier in cancer patients compared to healthy individuals, with a more pronounced effect in males. Additionally, individuals who later developed cancer had below-average B cell levels, indicating a potential marker for early disease detection.
Dr. Robert Bentham, the study’s first author, highlighted the novel approach of ImmuneLENS: “Unlike previous methods, which search for individual immune cell signals, our technique provides a broader view of immune cell distribution, offering new perspectives on disease progression and response to treatment.”
Potential for Personalized Cancer Treatment
The findings hold promise for enhancing immunotherapy, a treatment that leverages the body’s immune system to fight cancer. Since the proportion of T cells in a tumor is a known biomarker for treatment response, ImmuneLENS could help identify patients most likely to benefit from immunotherapy.
Dr. Nisharnthi Duggan, Research Information Manager at Cancer Research UK, underscored the significance of the study: “We are living in a golden age of research where sophisticated data analysis is shaping the future of cancer treatment. While further studies are necessary, this research paves the way for more personalized and effective cancer therapies.”
Looking Ahead
The next step for researchers is to integrate these biological markers into clinical practice. As ImmuneLENS can be implemented at no additional cost to current genetic testing procedures, it has the potential to become a routine component of cancer diagnosis and treatment planning.
With its ability to distinguish different B cell types and their role in tumor immunity, this method may also aid in the development of novel therapeutic targets. The study’s findings underscore the importance of systemic immune monitoring in cancer research, offering new hope for improved patient outcomes.
Disclaimer: This article summarizes scientific research and does not constitute medical advice. Patients should consult their healthcare providers for personalized medical guidance.