Situation at a glance
Description of the situation
On 7 January 2025, the International Health Regulations (IHR) National Focal Point (NFP) for the Plurinational State of Bolivia notified the World Health Organization (WHO) of one laboratory-confirmed human infection with Chapare virus (CHAPV) from one of the municipalities of La Paz Department. The patient is an adult male farmer in the age group of 50-60 years.
The patient developed symptoms including fever, headache, muscle pain, joint pain, and bleeding gums on 19 December 2024 and sought medical attention on 24 December. On 30 December, he was transferred to the local Health Center of the municipality due to worsening symptoms, where he died the same day. Blood samples were collected on 30 December before his death and sent to the National Center of Tropical Diseases (CENETROP), which confirmed CHAPV detection through real-time polymerase chain reaction (RT-PCR specific for CHAPV) testing on 2 January 2025.
An epidemiological investigation revealed significant risk factors for zoonotic disease transmission, including severe rodent infestation in and around the patient’s home. Environmental conditions such as wooden and corrugated metal housing, dirt floors, and peri-domestic coconut plantings created a conducive environment for rodent activity. The patient’s occupation as a farmer likely involved exposure to rodent burrows, further increasing the risk of infection.
Blood samples were collected from two close contacts of the case, which were negative. As of 13 January 2025, no secondary cases have been reported, and all identified contacts remain asymptomatic. Public health measures, including disinfection and rodent control, have been implemented, and investigations are ongoing. This is the fifth documented outbreak of Chapare haemorrhagic fever (CHHF) in Bolivia and globally since the virus was first identified in 2003.
Epidemiology
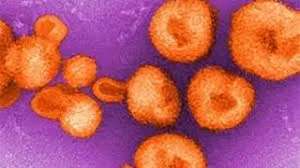
CHHF is a rare zoonotic disease caused by the CHAPV, a group of viruses belonging to the Mammarenavirus genus of the Arenaviridae family. These viruses are primarily transmitted to humans through infected rodents that serve as their natural hosts. Human transmission of Mammarenaviruses occurs mainly by inhalation of fine aerosol particles contaminated with virus-infected rodent excreta, such as urine, feces, or saliva. Human-to-human transmission is uncommon but has been documented, particularly in healthcare settings where infection prevention and control (IPC) measures are inadequate. This mode of transmission occurs through contact with the blood or bodily fluids of infected individuals and can be amplified during aerosol-generating medical procedures.
The incubation period ranges from 4 to 21 days, after which individuals may develop symptoms including fever, headache, muscle aches, vomiting, diarrhea, and in severe cases, haemorrhagic manifestations. Due to the nonspecific nature of early symptoms, CHHF can be challenging to diagnose, often requiring laboratory confirmation through methods like real-time polymerase chain reaction.
Currently, there is no specific antiviral treatment for CHHF; management focuses on supportive care to alleviate symptoms and maintain vital organ function. Case fatality rates for CHAPV infections range from 15% to 30% in untreated patients, with rates as high as 67% reported during outbreaks. Preventive measures emphasize reducing human exposure to rodent populations and implementing stringent IPC practices in healthcare settings to mitigate the risk of transmission.
CHHF is currently known to only occur in Bolivia. In the last 20 years, four outbreaks have been documented in the country. The first was reported in 2003 in Chapare Province, Cochabamba Department, involving a single fatal case. In 2019, a second outbreak occurred in La Paz Department, resulting in nine cases, including four deaths (case fatality rate: 60%). This second outbreak was caused by a different CHAPV strain than the one identified in 2003. The third outbreak took place in 2021 in La Paz Department, with three confirmed cases (two fatal). The most recent outbreak occurred in 2024 with one laboratory-confirmed case, also within La Paz Department.
Public health response
The local and national health authorities implemented the following public health measures:
- Epidemiological investigation: A field investigation was conducted, during which rodent feces were detected. These feces did not belong to the known transmitter (Rattus rattus). The rodent infestation rate was calculated and found to be 75%.
- Disinfection and rodent control: Disinfection measures and rodent control activities, including the use of rodenticides, were carried out both inside and outside the house.
- Community surveillance: Health personnel, in collaboration with the municipal vector control program, conducted follow-up with families residing in the neighboring area of the case, due to the presence of rodents in these locations.
- Community participation: Community engagement activities were carried out on 3 and 4 January 2025. These activities were planned by municipal and departmental health personnel to enhance awareness and participation in response efforts.
WHO risk assessment
One of the main challenges in detecting and responding to CHHF and other South American haemorrhagic fevers due to Mammarenavirus is the difficulty of making an early differential diagnosis due to the non-specificity of the initial clinical presentation. CHHF and other South American haemorrhagic fevers due to Mammarenavirus (e.g., Argentinian haemorrhagic fever, Bolivian haemorrhagic fever, and Sabia virus disease) should be considered for any patient presenting with suggestive symptoms originating from areas where Mammarenaviruses are known to circulate. These diseases should also be part of the differential diagnosis along with other endemic diseases such as malaria, dengue, yellow fever, and bacterial infections. Environmental exposures, such as evidence of rodent activity in or around the home, contact with rodent excreta, or visiting or working in areas where rodents are prevalent, should be carefully considered as key epidemiological risk factors. Case ascertainment should involve asking about exposure to rodents or contact with patients suspected of having haemorrhagic fevers due to Mammarenavirus. For biosafety reasons, all samples from suspected cases in regions where CHHF has previously been reported should be managed as Mammarenavirus samples, even for differential diagnosis.
In Bolivia, the geographical at-risk area is limited to rural areas in the northern part of the La Paz department, particularly along a jungle corridor from Caranavi to Teoponte municipalities, passing through the town of Palos Blancos, where the reservoir is found. Currently, CHHF is reported only in Bolivia. There is no significant risk of international spread of the disease, as person-to-person transmission of the Chapare virus is possible but remains rare in the general population. Continued surveillance, public awareness, and adherence to infection prevention and control measures are critical to preventing further spread and mitigating future outbreaks.
WHO advice
WHO recommends remaining vigilant and raising awareness among healthcare workers to detect, diagnose, and manage cases of haemorrhagic fever while ensuring strict compliance with infection prevention and control measures. Surveillance should focus on detecting suspected cases of haemorrhagic fever based on the clinical manifestations, travel history, and exposure history, tailored to the epidemiological context of the country or territory. Any individual who has had contact with the blood or bodily fluids of a suspected, probable, or confirmed haemorrhagic fever case during their illness is considered a contact. Contact monitoring should be performed for a maximum incubation period of 21 days following the last known exposure.
Laboratory confirmation of Mammarenavirus infection can be performed using various methods, including virological and serological techniques. However, the dynamics of Mammarenavirus infections (e.g., the duration of viraemia versus the appearance of antibodies) are not yet fully understood, and no serological assays have yet been validated for CHAPV. All biological samples should be treated as potentially infectious, handled only by trained personnel, and processed in suitably equipped laboratories.
Patients with suspected or confirmed CHHF should be isolated in a single room with a dedicated sink and toilet. Movement of patients with suspected or confirmed CHHF should be limited, however if patient ambulation outside of the room is necessary the patient should wear a medical mask during ambulation. All health and care workers in close contact with a patient with suspected or confirmed CHHF or who enter the isolation room should apply contact and droplet precautions, including the use of the following personal protective equipment: gown, examination gloves, medical mask, and eye protection (goggles or face shield). If an aerosol-generating procedure is performed on a patient with suspected or confirmed CHHF, the procedure should take place in a negative pressure airborne infection isolation room with the door closed. All health and care workers present in a room where an aerosol generating procedure is taking place should use airborne precautions in addition to contact and droplet precautions, including use of a fit-tested filtering facepiece respirator (e.g. N95).
Routine cleaning and disinfection of the isolation room of a patient with suspected or confirmed CHHF should occur three times daily, and spot cleaning should occur immediately whenever there is a spill or material contamination of blood or body fluids. Cleaning may be performed with soap and water applied by cloth, followed by disinfection with a 0.5% sodium hypochlorite solution; allowing the disinfectant to remain wet and untouched on the surface for a contact time of at least five minutes. All disposable waste that is generated in the patient room should be managed as infectious waste. Linens from isolation rooms are advised to be bagged and handled using contact precautions during transport to laundry areas and washed separately from other patient linens. Reusable medical equipment used on a patient with suspected or confirmed CHHF should be labelled as biohazardous and managed appropriately during transport and reprocessing in a medical device reprocessing department. Patients should be advised to place the lid down when flushing their dedicated toilet to avoid generating bioaerosols.
Ribavirin has been described as a treatment option for haemorrhagic fevers caused by some Mammarenaviruses; however, its efficacy and safety have not been demonstrated in randomized clinical trials. Supportive care, including hydration, rest, and treatment of complications, is recommended. Evaluation and management of co-infections such as malaria, dengue, yellow fever, or bacterial infections should also be considered.
Further information
- Control of Communicable Diseases. 21thEdition. Dr. David Heymann, Editor. 2022. American Public Health Association. Pag.44-47
- Toledo J., Paredes TorrezA., Alvaro Terrazas, Molina GutiérrezJ., Medina Ramírez A., Romero C., CondoriD., Alarcon de la Vega G., Swanson KortepeterM., Aldighieri S. Public health implications of a new world arenavirusoutbreak that occurred in Bolivia, 2019. Travel Medicine and InfectiousDisease. Vol 43, September – October 2021. Available: https://doi.org/10.1016/j.tmaid.2021.102124
- Pan American Health Organization/World Health Organization. Epidemiological Alert: Haemorrhagic fever due to Arenavirus in Bolivia. 18 July 2019. Washington, D.C. PAHO / WHO. 2019.Available from: https://www.paho.org/en/documents/epidemiological-alert-hemorrhagic-fever-due-arenavirus-bolivia-18-july-2019
- US Centers for Disease Control and Prevention(US CDC). About Chapare Haemorrhagic Fever. Available from: https://www.cdc.gov/chapare/about/index.html
- Loayza Mafayle R.,Morales-Betoulle ME., et al. (2022) Chapare Hemorrhagic Fever and Virus Detection in Rodents in Bolivia in 2019. The New England Journal of Medicine 386;24:2283-2294. Available from: https://www.nejm.org/doi/full/10.1056/NEJMoa2110339
- Plurinational State of Bolivia International Health Regulations National Focal Point.Email communication dated 7 January 2025. La Paz.; 2024. Unpublished.
- World Health Organization. Clinicalmanagement of patients with viral haemorrhagic fever: A pocket guide forfront-line health workers. Available from: https://www.who.int/publications/i/item/9789241549608
- World Health Organization Laboratory diagnosis of New World Arenavirus infection . Available in Spanish from: https://www.paho.org/es/documentos/diagnostico-por-laboratorio-infeccion-por-arenavirus-nuevo-mundo
- World Health Organization. Laboratory Systems. Available from: https://www.paho.org/en/topics/laboratory-systems
- World Health Organization. Transmission-based precautions (aide memoire). Available from: https://iris.who.int/handle/10665/356853
Citable reference: World Health Organization (20 January 2025). Disease Outbreak News; Chapare haemorrhagic fever in the Plurinational State of Bolivia. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2025-DON553