Outbreak at a glance
Dengue is endemic in Nepal. The country is experiencing a surge in cases that started from the week commencing 8 August to 26 August. Between January to 28 September 2022, a total of 28 109 confirmed and suspected dengue cases and 38 confirmed deaths due to dengue have been recorded, affecting all seven provinces. The causative serotype(s) is unknown. This represents the largest dengue outbreak in Nepal with regard to the cumulative number of cases reported nationwide per year.
Description of the outbreak
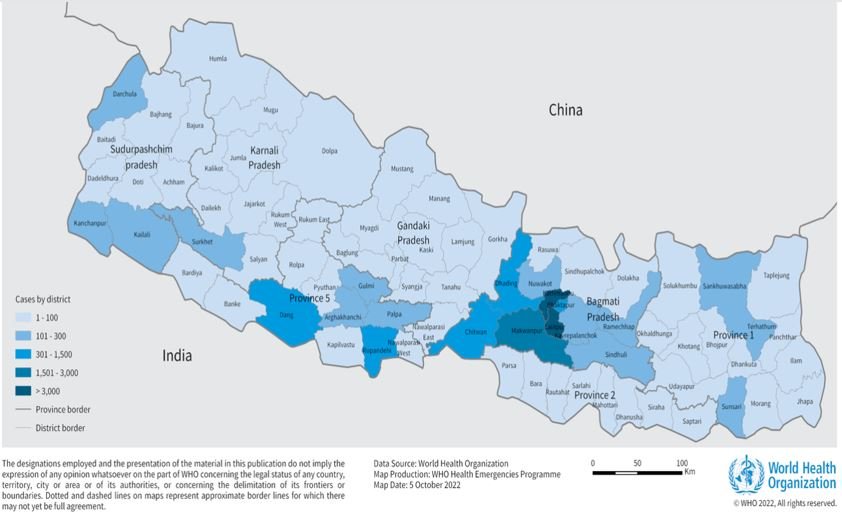
Between January and 28 September 2022, a total of 28 109 suspected and confirmed cases of dengue fever including 38 confirmed deaths (overall CFR 0.13%) have been reported from all seven provinces of Nepal, affecting all 77 districts in Nepal (Figure 1). Bagmati province which is the second-most populous province has reported the highest number of cases (78.2%) and deaths (68.4%).
According to the Epidemiology and Disease Control Division (EDCD) of the Ministry of Health and Population, the highest number of new cases in 2022 have been reported in the districts of Kathmandu (n=9528; 33.8%), Lalitpur (n=6548; 23.2%), and Makwanpur (n=2776, 9.8%).
Data on demographics was available for 23% of cases (n= 6734) of which 76% (5175/6734) were aged 15-59 years old, and 54% were males (n=3637). As of 28 September, 38 deaths have been verified, of which males and cases aged 15 – 59 years old each accounted for 55% (n=21) of reported deaths. Cases aged over 60 years old accounted for 39% (n=15) of reported deaths.
Dengue cases have increased since July coinciding with the rainy season with majority of the cases reported during September (83.6%; n=23 514).
Figure 1. Number of Dengue cases reported from districts of Nepal from 1 January- 28 September 2022. 
Figure 2. Number of dengue cases reported by months in Nepal from 1 January to 28 September 2022 
Epidemiology of the disease
Dengue is a viral infection transmitted to humans through the bite of infected mosquitoes and is found in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. The primary vectors that transmit the disease are Aedes aegypti mosquitoes and, to a lesser extent, Aedes albopictus.
Dengue virus (DENV) has four serotypes (DENV-1, DENV-2, DENV-3, DENV-4) and it is possible to be infected by each. Infection with one serotype provides long-term immunity to the homologous serotype but not to the other serotypes; sequential infections put people at greater risk for severe dengue. Many DENV infections produce only mild illness; over 80% of cases are asymptomatic. DENV can cause an acute flu-like illness.
There is no specific treatment for dengue; however, timely detection of cases, identifying any warning signs of severe dengue infection, and appropriate case management are key elements of care to prevent patient death and can lower fatality rates of severe infection to below 1%.
Public health response
The Epidemiology and Diseases Control Division of the Ministry of Health and Population initiated the following actions to manage and coordinate the response:
- Overall response: The Ministry of Health and Population (MoHP) together with WHO and hospitals convened a meeting to review the preparedness and map out strategic interventions for the dengue outbreak in the country. Virtual meetings have been conducted with provinces, districts, and local levels of the MoHP to review the current epidemiology and the responses required. WHO drafted the multisectoral engagement plan to accelerate the Dengue Response and submitted it to the EDCD for review and implementation of action plans.
- Vector Control measures: WHO assisted in the development of a standard operating procedure for vector control activities. Technical working group meetings have been convened to facilitate dengue response and to strengthen vector surveillance activities in high-risk/high-case reporting districts in Kathmandu valley (which is in Bagmati province) and Lumbini province). Search and destroy campaigns for mosquitoes in municipalities including Lalitpur and Kathmandu (prioritizing main breeding containers) have been initiated. Vector surveillance and sample collection in high-case reporting districts in Kathmandu have been initiated.
- Laboratory: A total of 39 000 diagnostic kits have been provided through WHO and Government funding. WHO facilitated sample collection for serotyping from ten identified hospitals nation wise in collaboration with EDCD and National Public Health Laboratory (NPHL).
- Clinical Management: A total of 200 physicians and medical officers were trained in September, in the case management of dengue fever, referral of dengue patients, and reporting for the dengue surveillance system. This included in-person attendance of 70 healthcare workers (HCWs) from major hospitals in Kathmandu Valley and an additional 130 HCWs from all Provinces who joined virtually. The video recording of the orientation has been disseminated by EDCD for its wider use.
WHO risk assessment
Nepal reported its first dengue case in a traveller returning from India in 2004. Since then, dengue has been endemic in Nepal. The country has expertise and experience in managing dengue, however, WHO considers the overall risk for the current dengue outbreak high at the national level due to the following reasons:
- As dengue is recurrent in the country, the population may be at risk of re-infection and therefore, serious complications may occur if not managed promptly and correctly. At present, severe dengue cases and case-fatality rates appear to be increasing, likely due to the limited hospital capacity in-country and limited access to and use of health care services. With the current increase in other vector-borne diseases in Nepal this year, such as Japanese Encephalitis and Scrub typhus, affecting the national health system capacity, there is a high risk of serious health impacts from dengue fever.
- Dengue virus has the potential to cause epidemics resulting in high morbidity and mortality. There is no specific treatment. Early recognition of dengue virus infection and appropriate clinical management can reduce the severity of disease and mortality among dengue patients.
- The current circulating serotype is unknown at this stage, although further laboratory tests are planned. Infection with one serotype provides long-term immunity to the homologous serotype, however, the risk for severe dengue is high in a second infection with a different DENV serotype.
- Current data suggests that dengue cases are increasing in magnitude and expanding out of the lowland areas typically suitable for the breeding of Aedes mosquitoes to higher elevations, potentially due to climate changes and rapid urbanization.
This outbreak underscores the need for improved vector surveillance, enhanced laboratory capacity for better case detection, and improved surveillance of acute febrile illness in Nepal to effectively control the outbreak.
There is frequent population movement across the Nepal-India land border. Dengue is endemic in many parts of India including northern Indian States, which share the border with Nepal. Given the high incidence in Nepal, it is possible that dengue may spread across the border into India, although its consequences may depend on a number of factors such as the density of vectors, circulating serotypes, and level of public health response in the neighbouring Indian states. Nepal is a popular tourist destination, hence, spread through international travellers cannot be ruled out as Nepal is easing international travel restrictions imposed in response to COVID-19.
WHO advice
The proximity of mosquito vector breeding sites to human habitation is a significant risk factor for dengue virus infection. Although dengue does not spread from human to human, mosquitoes can become infected after biting infected individuals. This cycle, therefore, makes the infected mosquito capable of spreading the dengue virus among households and in the neighbourhood, leading to clusters of cases.
The prevention and control of dengue depend on effective vector control. WHO promotes a strategic approach known as Integrated Vector Management (IVM) to control mosquito vectors, including Aedes subspecies (the vector of dengue). IVM should be enhanced to remove potential breeding sites, reduce vector populations, and minimize individual exposure. This should involve vector control strategies for larvae and adults (i.e., environmental management and source reduction, and chemical control measures), as well as strategies for protecting people and households.
Vector control activities should focus on all areas where there is a risk of human-vector contact (place of residence, workplaces, schools and hospitals, and construction sites in Kathmandu Valley). Vector control activities can include covering, draining, and cleaning household water storage containers on a weekly basis. Space spraying with insecticide can be deployed as an emergency measure. Chlorination and application of suitable larvicides/insecticides for water storage in outdoor containers should also be considered.
Personal protective measures during outdoor activities include the application of repellents to exposed skin or clothing, and the wearing of long sleeves shirts and trousers. Indoors, additionally, protection can include the use of household insecticide aerosol products or mosquito coils. Window and door screens, as well as air conditioning, can reduce the probability of mosquitoes entering the house. Insecticide-treated nets offer good protection to people against mosquito bites while sleeping during the day. Since Aedes mosquitoes are active at dawn and dusk, personal protective measures are recommended particularly at these times of the day.
There is no specific treatment for dengue infection, but early detection of warning signs and timely access to appropriate clinical management (including referral to an appropriate health care facility) reduce the risk for severe dengue complications and mortality. Vector and human case surveillance should continue to be enhanced in all affected areas and across the country. Where feasible, resources should be allocated for the strengthening of a sample referral mechanism for the confirmation and sub-typing of dengue virus.
WHO does not recommend that any general travel or trade restrictions be applied to Nepal based on the information available for this event.
Further information
- WHO factsheet: Dengue and severe dengue
- WHO Q&A: Dengue and severe dengue
- WHO Health topics: Dengue and severe dengue
- WHO Dengue control strategies
- Global Strategy for dengue prevention and control, 2012–2020
- Strong country capacity, improved tools and community engagement critical to enhancing dengue prevention and control
Citable reference: World Health Organization (10 October 2022). Disease Outbreak News; Dengue fever – Nepal. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON412