Long COVID continues to present a puzzle, with its varied symptoms and manifestations. Researchers are in pursuit of concrete answers due to the condition’s recent emergence and diverse symptomatology. Understanding the mechanisms behind long COVID could pave the way for more effective treatments from healthcare providers.
Recent research indicates that individuals with rheumatic disease and a prior OC43 cold virus infection are at a heightened risk of developing long COVID. This revelation also suggests that OC43 antibodies in the bloodstream could serve as a biomarker for identifying those predisposed to experiencing long COVID, also known as post-acute sequelae of coronavirus disease 19.
Dr. Zachary Wallace, a co-author of the study and a rheumatologist at Massachusetts General Hospital, explains, “Patients with rheumatic disease may be predisposed to long COVID because of their dysregulated immune responses from their disease and/or its treatments.” The unique autoimmune responses, fibrosis, and other pathological processes inherent to individuals with rheumatic disease make them a pertinent population for initial evaluation.
Published on September 6 in Science Translational Medicine, these findings may extend beyond rheumatic patients. Dr. Wallace suggests, “The findings observed in patients with rheumatic disease could be unique to this population but may be shared among people without rheumatic disease who develop long COVID.”
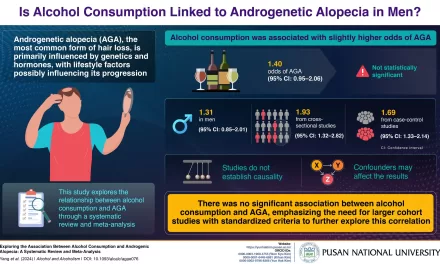
Both OC43 and SARS-CoV-2 belong to the betacoronavirus family, creating a familial link. In individuals with a history of OC43 common cold, their immune system may misidentify a subsequent COVID infection as OC43, mounting a defense against the wrong virus. This partial protection against COVID renders them more susceptible to long COVID.
Dr. Jeffrey A. Sparks of Brigham and Women’s Hospital emphasizes, “Our findings suggest that an enriched response to OC43 may be associated with worse outcomes.” This implies that those whose immune systems treat COVID as a wholly new infection might fare better.
The connection between prior OC43 cold and subsequent long COVID was unexpected. Wallace states, “We initially expected that immune response to SARS-CoV-2 would be the most important marker and did not necessarily expect immune response to different pathogens to be as important contributors.”
While creating a serum biomarker based on antibody levels is technically feasible, Wallace notes the need for replication in diverse populations and under current COVID circumstances. The specific threshold of OC43 antibodies indicating elevated risk remains unclear.
Dr. Fernando Carnavali of Mount Sinai Center for Post-COVID Care applauds the study, emphasizing its significance for patients seeking clarity about long COVID. However, he advises caution due to the relatively small participant pool, highlighting the need for further research.
Dr. Oladunni Adeyiga, part of a multidisciplinary team treating long COVID patients, expresses enthusiasm for the study’s insights into the underlying mechanisms. She emphasizes the importance of understanding why long COVID occurs to inform potential therapeutic interventions.