At the University of Mississippi, a bowl of free condoms sits near the gym entrance, often overlooked by passing students. Though campus officials refill the bowl several times daily, most students simply pass by, giggling or dismissing the offer. This casual disregard for condoms reflects a broader trend among younger generations in the U.S.: despite widespread availability, condom usage has declined significantly.
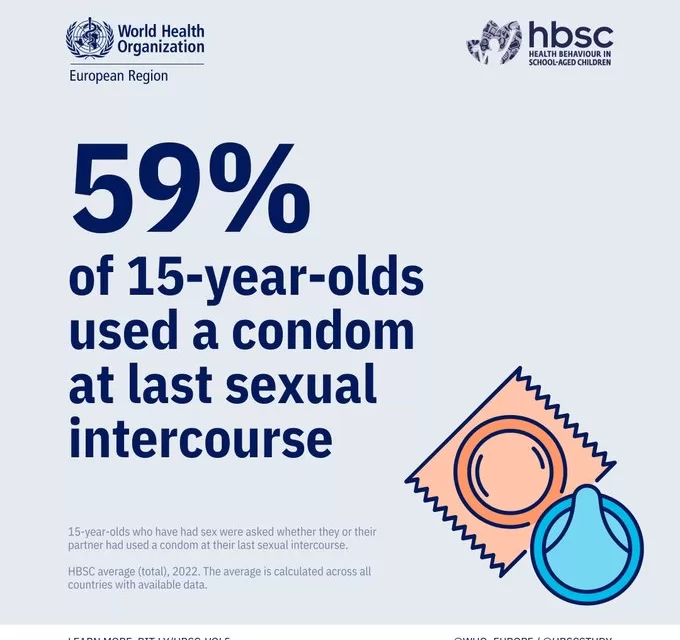
While fewer teens and young adults are sexually active today, those who are sexually active are less likely to use condoms, even as rates of sexually transmitted infections (STIs) remain high. In 2022, young people aged 15 to 24 accounted for half of all new cases of chlamydia, gonorrhea, and syphilis, according to public health officials.
The decline in condom use stems from multiple factors, including the availability of long-term birth control options and drugs like pre-exposure prophylaxis (PrEP) that prevent HIV. Additionally, varying levels of sex education across the country have left some students with limited knowledge of safe sex practices, further contributing to the decline.
A Shift in Condom Use Attitudes
For many students, condoms have become an afterthought. “Using a condom is just a big, ‘uh, no,’” says Magan Perry, president of the Public Health Student Association at Ole Miss. She notes that women often have to initiate condom use in relationships, and many men resist, offering alternative solutions like emergency contraception or simply dismissing the need for protection.
This shift is not limited to heterosexual relationships. Among men who have sex with men, condom use has also declined as the fear of contracting HIV has lessened with the rise of PrEP. Dr. Joseph Cherabie, medical director of the St. Louis HIV Prevention Training Center, notes that earlier condom advertisements often relied on fear to encourage use, but today’s messages are shifting toward personalized prevention strategies.
While condoms were once seen as a critical line of defense, they now seem to be overshadowed by medical advancements. Dr. Steven Goodreau, an HIV expert at the University of Washington, worries that the promotion of PrEP is diminishing condom use as a preventative strategy, especially among younger generations. He points out that federal HIV research plans and the national “Ending the HIV Epidemic” initiative no longer prominently mention condoms, despite their proven effectiveness.
Medical Advances Expand Options
The landscape of STI and pregnancy prevention has evolved with the development of new medical tools. Many young women have turned to long-term contraceptive methods like intrauterine devices (IUDs) and birth control pills, reducing their reliance on condoms. Advances in STI prevention are also emerging, such as doxycycline post-exposure prophylaxis (doxy PEP), a drug that can prevent bacterial STIs like chlamydia, gonorrhea, and syphilis when taken within 72 hours of unprotected sex.
These medical options have allowed individuals to feel more secure about their sexual health without using condoms, but public health experts are quick to emphasize that condoms still play an important role in preventing HIV and other STIs. “Condoms are effective when used consistently and correctly,” says Dr. Bradley Stoner, director of the CDC’s Division of STD Prevention.
The Role of Sex Education
One of the underlying causes of declining condom use is the variability in sex education across the U.S. In states like Mississippi, abstinence-focused curricula dominate public schools, often leaving students with limited knowledge about contraception and safe sex practices. Condom demonstrations are banned in Mississippi classrooms, and sex education programs are either abstinence-only or abstinence-plus, meaning condoms are mentioned but not promoted.
In contrast, states like Oregon have comprehensive sex education programs that provide students with medically accurate information and practical skills, such as how to properly use a condom. These differences in educational standards contribute to stark contrasts in attitudes toward condoms between students from different regions.
The lack of uniform sex education nationwide has left many young people unprepared to make informed decisions about their sexual health. Advocates like Michelle Slaybaugh, director of social impact and strategic communication for the Sexuality Information and Education Council of the United States, believe comprehensive sex education is essential to equipping young adults with the tools they need to protect themselves.
A Call for Change
As condom use continues to decline, public health experts are faced with the challenge of finding new ways to encourage safe sex practices among young people. Dr. Cherabie emphasizes the need for a balanced approach that includes both new medical advancements and traditional methods like condoms. “We have to plan for the fact that people will choose to have condomless sex,” he says, “but we also need to ensure they are aware of all their options.”
In a time of rapid medical progress, condoms remain a critical, accessible tool for preventing STIs. Public health efforts must adapt to changing attitudes and ensure younger generations are educated and empowered to make informed choices about their sexual health.