Situation at a glance
On 11 July 2023, WHO received an official report regarding the detection of a circulating vaccine-derived poliovirus type 2 (cVDPV2) in two acute flaccid paralysis (AFP) cases and two asymptomatic healthy children community contacts from Hagadera refugee camp, in Kenya, the second largest refugee camp in the world with over 100 000 refugees.
The genetic sequencing analyses showed that all four isolates are genetically linked to the cVDPV2 circulating in Banadir, Somalia.
WHO assesses the overall risk at the national level to be high due to the overcrowded living conditions in the refugee camp, high rate of malnutrition, poor water and sanitation facilities, and frequent population movements with Somalia.
Description of the situation
On 11 July 2023, WHO received an official report regarding the detection of circulating vaccine-derived poliovirus type 2 (cVDPV2) in Kenya. The detection was reported from Hagadera refugee camp which is the second largest refugee camp in the world with over 100 000 refugees.
Four genetically-linked cVDPV2 were isolated in samples from two acute flaccid paralysis (AFP) cases, and two asymptomatic healthy children community contacts, from Fafi district, Garissa county. The cases and community contacts are all from Hagadera refugee camp, associated with frequent population movement with neighboring Somalia.
The first case is a 2-year-old male, vaccinated with three doses of oral poliovirus vaccine (OPV), with no travel history, who developed paralysis on 26 May, and stool samples were collected on 1 June and 2 June. The second case is a 2.7-year-old female with a travel history to Afmadhow, Lower Juba, southern Somalia, vaccinated with three doses of oral polio vaccine (OPV) who developed paralysis on 27 May, and stool samples were collected on 2 June and 3 June 2023.
A community contact, a 2-year-old male asymptomatic healthy child was identified with a stool sample collected on 25 May 2023. The child has zero-dose vaccination. A second asymptomatic healthy child community contact was also identified from Hagadera refugee camp with the same emerging strain from Somalia and case investigation is being conducted.
The genetic sequencing analyses showed that all four isolates have undergone between 65 and 73 nucleotide changes from Sabin and are genetically linked to the cVDPV2 circulating in Banadir, Somalia.
According to the WHO UNICEF estimates of national immunization coverage, oral polio vaccine third dose (OPV3) and inactivated poliovirus vaccine first dose (IPV) was 91% in Kenya in 2021. However, the coverage in Hagadera camp is 77% for both OPV3 and IPV as of May 2023.
Epidemiology of Poliomyelitis
Polio is a highly infectious disease that largely affects children under five years of age, causing permanent paralysis (approximately 1 in 200 infections) or death (2-10% of those paralyzed).
The virus is transmitted from person-to-person, mainly through the fecal-oral route or, less frequently, by a common vehicle (e.g., contaminated water or food) and multiplies in the intestine, from where it can invade the nervous system and cause paralysis. The incubation period is usually 7-10 days but can range from 4-35 days. Up to 90% of those infected are either asymptomatic or experience mild symptoms and the disease usually goes unrecognized.
Vaccine-derived poliovirus is a well-documented strain of poliovirus mutated from the strain originally contained in OPV. OPV contains a live, weakened form of poliovirus that replicates in the intestine for a limited period, thereby developing immunity by building up antibodies. On rare occasions, when replicating in the gastrointestinal tract, OPV strains genetically change and may spread in communities that are not fully vaccinated against polio, especially in areas where there is poor hygiene, poor sanitation, or overcrowding. The lower the population’s immunity, the longer this virus survives and the more genetic changes it undergoes.
In very rare instances, the vaccine-derived virus can genetically change into a form that can cause paralysis as does the wild poliovirus – this is what is known as a vaccine-derived poliovirus (VDPV). The detection of VDPV in at least two different sources and at least two months apart, that are genetically linked, showing evidence of transmission in the community, is classified as ‘circulating’ vaccine-derived poliovirus type 2 (cVDPV2).
Public health response
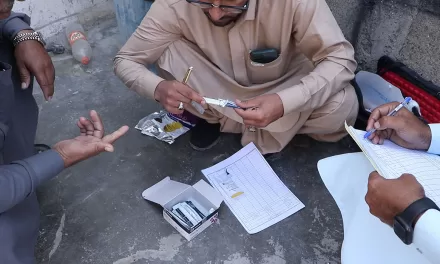
- The Ministry of Health (MoH), with support from the Global Polio Eradication Initiative partners have conducted a risk assessment, along with a field investigation.
- The MoH, through the Division of Disease Surveillance and Response and the Public Health Emergency Operations Centre, has activated a Technical Coordination Committee to begin preparations for the implementation of emergency outbreak response, as per internationally-agreed outbreak response guidelines, including rapid implementation of large-scale supplementary immunization activities, with the most appropriate, available type-2 containing polio vaccine.
- Sub National Immunization Days (SNIDs) with nOPV2 have been planned as part of the rapid response; the first round of the vaccination campaign in August will vaccinate all children under 5 years of age targeting Garissa county, the epicenter of the outbreak, and neighboring counties with a Somali community as well as Nairobi (the capital), due to population movements. A second and third round with the expansion of targeted areas is being planned to be conducted in September and October.
- Active surveillance for additional AFP cases is being further strengthened, consideration is being given to establishing new environmental sites, cross border surveillance is being intensified, and subnational immunity levels are being analyzed to identify potential un- or under-immunized populations and/or areas.
WHO risk assessment
The MoH established the Kenya Expanded Programme on Immunization (KEPI) for six priority diseases including polio in 1980.
Inactivated polio vaccine was introduced in 2015. Although the country did not have a wild poliovirus outbreak in 2014, Kenya, together with other Horn of African countries remained at risk of imported wild poliovirus from neighbouring Somalia due to the 2013 outbreak that continued until July 2014. After this polio outbreak in 2013, the country initiated environmental surveillance for polioviruses in an effort to supplement AFP surveillance, which is the benchmark for surveillance of wild poliovirus.
WHO assesses the overall risk at the national level to be high due to the overcrowded living conditions in the refugee camp, high rate of malnutrition, poor water and sanitation facilities, mass and frequent population movements with Somalia, influx of new arrivals to the camp, late identification of the newly arrived children, high prevalence of zero dose children among the newly arriving children from middle and lower Juba Somalia, and sub-optimal surveillance performance.
WHO considers the risk of international spread and/or emergence of cVDPV2 of this strain to be high, particularly across other areas of the Horn of Africa, due to the low population immunity, the use of trivalent OPV (tOPV) in Somalia, suboptimal surveillance, and inadequate routine immunization levels in some areas, and large-scale population movements.
In all instances, the continued spread of existing outbreaks including the genetically linked cVDPV2 cases detected in Kenya which is genetically linked to the one circulating in Somalia as well as the emergence of new outbreaks of cVDPV2 indicates significant gaps in routine immunization coverage and inadequate outbreak response vaccination. The risk of further spread of such strains, or the emergence of new strains, is exacerbated by decreased immunization rates related to disruption in routine and campaign immunization during the COVID-19 pandemic.
WHO advice
It is important that all countries, particularly those with frequent travel and contacts with polio-affected countries and areas, strengthen surveillance for AFP cases and commence planned expansion of environmental surveillance to rapidly detect any new virus importation and facilitate a rapid response. Countries, territories and areas should also maintain uniformly high routine immunization coverage at the district level, including vulnerable populations such as Refugees/Returnees to minimize the consequences of any new virus introduction.
WHO’s International Travel and Health recommends that all travelers to polio-affected areas be fully vaccinated against polio. Residents (and visitors for more than 4 weeks) from infected areas should receive an additional dose of OPV or IPV within 4 weeks to 12 months of travel.
As per the advice of an Emergency Committee convened under the International Health Regulations (2005), the risk of international spread of poliovirus remains a Public Health Emergency of International Concern (PHEIC). Countries affected by poliovirus transmission are subject to Temporary Recommendations. To comply with the Temporary Recommendations issued under the PHEIC, any country infected by poliovirus should declare the outbreak as a national public health emergency, ensure the vaccination of residents and long-term visitors and restrict at the point of departure travel of individuals, who have not been vaccinated or cannot prove the vaccination status.
The latest epidemiological information on cVDPVs is updated on a weekly basis.
Further information
- Global Polio Eradication Initiative
- Poliomyelitis Fact sheets
- WHO immunization dashboard
- GPEI Public health emergency status
- International travel and health
- Vaccine-derived polioviruses
- GPEI country page for Kenya
- Kenya Comprehensive Multi-Year Plan for Immunization
- UNHCR Hagadera Refugee camp
Citable reference: World Health Organization (28 July 2023). Disease Outbreak News; Circulating vaccine-derived poliovirus type 2 (cVDPV2) in Kenya. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON479