Cholera is endemic in Somalia with recurrent outbreaks reported since 2017. Between 1 January to 10 July 2022, a cumulative number of 7796 cases of cholera including 37 associated deaths (case fatality ratio 0.5%) have been reported from 25 drought-affected districts.
The current cholera outbreak is taking place in the context of other ongoing outbreaks, high rates of malnutrition, and the escalating drought, all of which are exacerbating the fragility of Somalia’s humanitarian situation and have led to large displacement of people, placing additional pressure on an already over-burdened and underperforming healthcare system. Currently, the country has limited capacity to respond to the outbreak, increasing the risk of serious public health impact.
Description of the outbreak
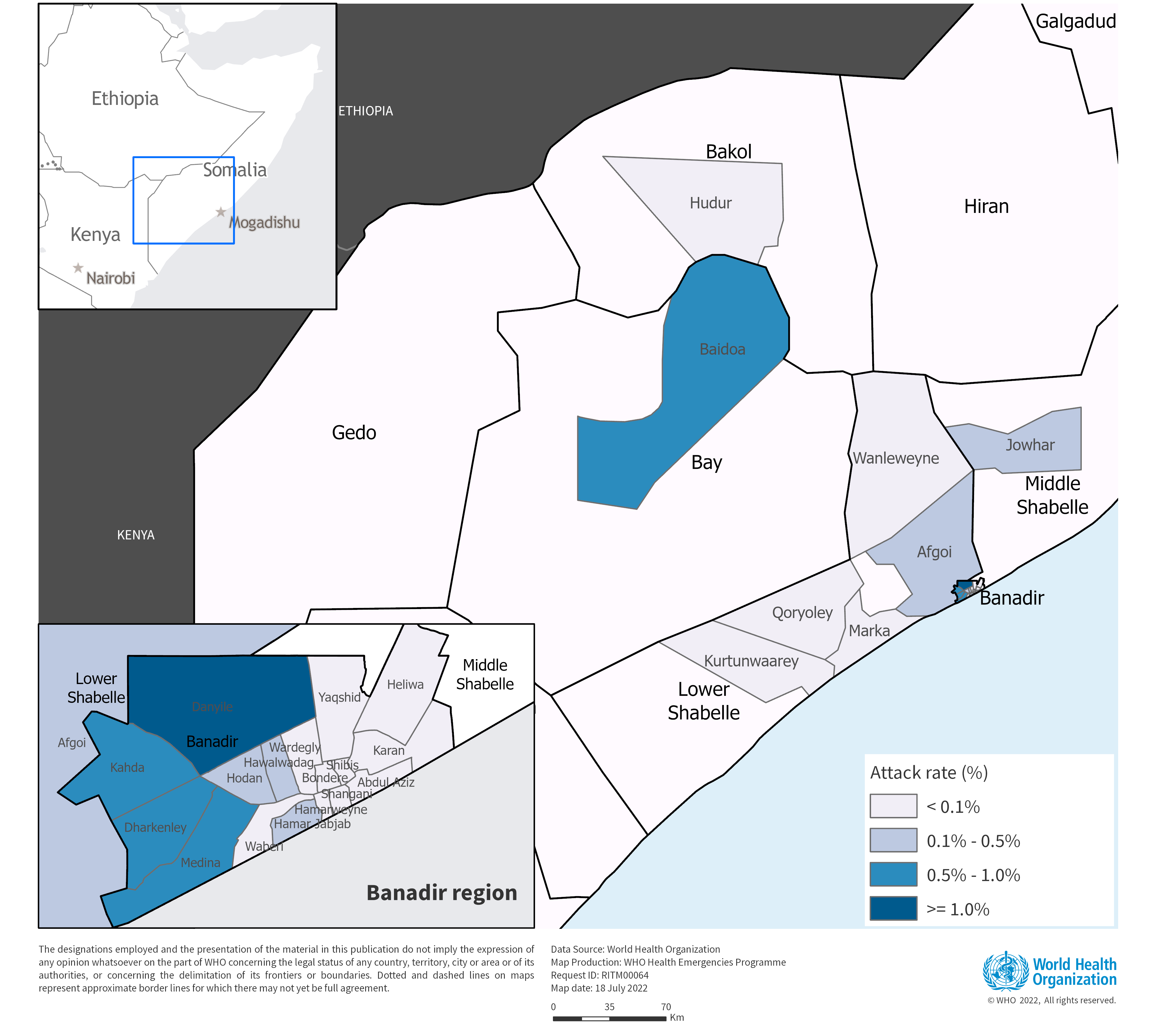
From 1 January to 10 July 2022, according to the Ministry of Health Somalia (MOH), a cumulative number of 7796 cases of cholera including 37 associated deaths (CFR: 0.5%) have been reported from 25 drought-affected districts in Banadir region, South-West state and Hirshabelle state (Table-1). The districts reporting the highest number of cases include Baidoa (2033), Daynile (1080), Jowhar (825) and Afgoi (681). In addition to being the drought-affected districts, many of these districts also host Internally Displaced Populations (IDP) in camps resulting from three decades of conflict and the escalating drought situation.
Over half of the cases (53.5%) were among children below two years of age, with males and females equally affected. Severe dehydration was reported in 27% of cases. None of the cases reported having received Oral Cholera Vaccine (OCV). OCV campaigns were carried out in Somalia in 2017, 2018 and 2019.
As of 10 July, a total of 677 stool samples were collected and analyzed (by culture) by the National Public Health laboratory in Mogadishu. Of these, 145 samples (21.4%) tested positive for Vibrio cholerae Ogawa 01.
The number of cases reported in the first six months of 2022 has exceeded the number of cases reported in 2021 in the same drought affected districts, when a total of 6205 acute watery diarrhoea (AWD)/suspected cholera cases including 39 deaths (CFR:0.63%) were reported. In 2021, the outbreak started following flash floods.
Table-1: Number of cholera cases, deaths, case fatality ratios and attack rates by districts in Somalia; from 1 January to 10 July 2022(epidemiological week 1-27, 2022)
Figure: 1- Geographic distribution of cholera cases in Somalia (%) from 1 January to 10 July 2022
Figure 2: Number of suspected cholera cases in Somalia reported from 1 January 2021 through 10 July 2022
Epidemiology of cholera
Cholera is an acute enteric infection caused by ingesting the bacteria Vibrio cholerae present in contaminated water or food. It is mainly linked to insufficient access to safe drinking water and inadequate sanitation. It is an extremely virulent disease that can cause severe acute watery diarrhoea resulting in high morbidity and mortality, and can spread rapidly, depending on the frequency of exposure, the exposed population and the setting. Cholera affects both children and adults and can be fatal if untreated.
The incubation period is between 12 hours and five days after ingestion of contaminated food or water. Most people infected with V. cholerae do not develop any symptoms, although the bacteria are present in their faeces for 1-10 days after infection and are shed back into the environment, potentially infecting other people. Among people who develop symptoms, the majority have mild or moderate symptoms, while a minority develop acute watery diarrhoea with severe dehydration. Cholera is an easily treatable disease. Most people can be treated successfully through prompt administration of oral rehydration solution (ORS).
Cholera can be endemic or epidemic. A cholera-endemic area is an area where confirmed cholera cases were detected during the last three years with evidence of local transmission (cases are not imported from elsewhere). A cholera epidemic can occur in both endemic countries and in non-endemic countries. Uninfected dead bodies have never been reported as the source of epidemics.
The consequences of a humanitarian crisis – such as disruption of water and sanitation systems, or the displacement of populations to inadequate and overcrowded camps – can increase the risk of cholera transmission, should the bacteria be present or introduced.
A multisectoral approach including a combination of surveillance, improving access to clean water, sanitation, and hygiene promotion, rapid access to treatment, risk communication and community engagement and oral cholera vaccines is essential to control cholera outbreaks and to reduce deaths.
Public health response
Emergency response activities are being conducted by the MOH, WHO and other partners. These measures include:
- The use of an Incident Management System at the national level to coordinate drought response including cholera response activities.
- A Cholera Task Force was established to coordinate the implementation of cholera response activities including the implementation of reactive OCV campaigns.
- The first round of reactive oral cholera vaccination campaign was conducted (14-26 June 2022) in the nine high-risk districts and 897 086 (96%) of the people aged one year and above including pregnant women have been vaccinated against cholera.
- Activation of an Early Warning Alert and Response Network (EWARN) in drought affected districts is ongoing including community health workers who detect and report community alerts.
- Deployment of district based rapid response teams to investigate alerts of acute watery diarrhoea (AWD) reported from health facilities and communities.
- Provision of state-based laboratories with reagents and other relevant supplies for the confirmation of cholera cases.
- Prepositioning of essential supplies for the detection of suspected cholera by rapid diagnostic test (RDTs) and the management of cholera cases in remote communities.
- Health sensitization sessions targeting people living in IDP camps conducted by health cluster partners along with the MOH.
- Implementation of water, sanitation and hygiene (WASH) interventions including the distribution of hygienic kits to displaced communities are ongoing.
- WASH cluster, in collaboration with MOH, is conducting water quality monitoring and chlorination of contaminated water sources.
- Hygiene kits have been distributed to districts reporting high numbers of cases.
- Six cholera treatment centres have been established in high-risk districts.
WHO risk assessment
In 2017, more than 78 000 suspected cholera cases including 1159 deaths (CFR 1.5%) were reported in Somalia. Transmission has continued since, with 6761 suspected cholera cases and 45 deaths (CFR 0.67%) reported in 2018; 3100 cases and four deaths (CFR 0.13%) reported in 2019; 6414 cases and 44 deaths (CFR 0.69%) reported in 2020 and 6205 AWD/cholera cases and 39 deaths (CFR 0.63%) reported in 2021.
The current cholera outbreak in Somalia is taking place in the context of other ongoing outbreaks (including COVID-19, measles), as well as the escalating drought that has affected seven million people and displaced 805 000 people to camps according to the United Nations Office for the Coordination of Humanitarian Affairs (UNOCHA), putting pressure on an already overstretched health-care system with limited primary healthcare services. The Somalia Food Security and Nutrition Unit has reported that multiple areas face a risk of famine during the current drought and under escalating food prices with more than 45% of the population classified as Integrated Food Insecurity Phase Classification (IPC) 3 (Crisis) [1] and more. The drought has further stretched response capacity in Somalia.
Additionally, the current cholera outbreak has been confirmed in 25 drought affected districts, which hosts displaced communities who have limited access to safe water, proper sanitation and access to food.
Although there is currently no evidence of cross-border spread of the outbreak, international spread cannot be ruled out given the escalating drought conditions across the Horn of Africa, which has led to repeated displacement and extensive cross-border population movement between Somalia and nearby countries especially Ethiopia, Kenya, Djibouti and Yemen. These countries are also experiencing similar conditions (limited access to safe water, proper sanitation and food) that may facilitate the transmission of diarrheal disease, especially affecting displaced communities.
WHO advice
WHO recommends strengthening of disease surveillance systems, and proper and timely case management of cholera cases. Oral cholera vaccines should be used in conjunction with improvements in water and sanitation to control cholera outbreaks and for prevention in areas known to be at high risk for cholera. Improving access to safe drinking water and sanitation infrastructure, as well as improving infection, prevention and control in healthcare facilities, with hygiene practices and food safety in affected communities, are the most effective means of controlling cholera. Key public health communication messages should be provided to the population.
Specifically, in Somalia, despite ongoing response activities there is an urgent need to reinforce the following actions in drought affected districts:
- Deploy additional district rapid response teams and community health workers to detect and report alerts and conduct risk communication.
- Build the capacity of frontline health workers in clinical management of cholera cases.
- Preposition of cholera kits.
- Establish Oral Rehydration Points (ORPs) in the affected communities, supporting linkages of ORPs to Cholera Treatment Centers (CTCs).
- Scale-up of community awareness and sensitization campaigns.
- Strengthening the implementation of WASH interventions in drought affected districts.
- Develop an updated cholera response plan to stream line coordination for cholera response.
WHO does not recommend any travel or trade restrictions for Somalia based on the currently available information.
Further information
- WHO Cholera fact sheet
- WHO Disease outbreak news: Cholera Somalia 29 March 2018
- Weekly Epidemiological Record 2016
- Weekly Epidemiological Record 2017
- Weekly Epidemiological Record 2019
- Weekly Epidemiological Record 2020
Citable reference: World Health Organization (20 July 2022). Disease Outbreak News; Cholera in Somalia. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON398