Situation at a glance
Cholera is endemic in the eastern part of the Democratic Republic of the Congo (DRC), including Ituri, North Kivu, South Kivu, and Tanganyika provinces, with cases reported through the year.
On 14 December 2022, a cholera epidemic was officially declared by the Governor of the province of North Kivu, following the isolation of Vibrio cholerae among 140 of the 247 samples collected from suspected cases of Nyiragongo HZ.
As of 4 February 2023, a total of 4386 cholera cases (of which 1009 are laboratory-confirmed) with 16 deaths (CFR 0.4%) have been reported.
A multisectoral community-based response has been implemented, including a cholera vaccination campaign.
Considering the fragile context in which this outbreak is taking place, ongoing armed conflicts with further displacements, concurrent epidemics, inadequate levels of access to health care, poor drinking water, hygienic and sanitary conditions, and population movements between the affected HZs and neighbouring countries (including Rwanda and Uganda), WHO assesses the risk posed by this outbreak as high at the national and regional level, and low at the global level.
Description of the situation
Cholera is endemic in several provinces in the Democratic Republic of the Congo (DRC).
However, from mid-November to the end of 2022, there has been an upsurge in the number of reported cholera cases in the health zones of Nyiragongo and Karisimbi, in the province of North Kivu. Since then, cases have shown a declining trend (Figure 1).
Figure 1. Number of cholera cases (suspected and confirmed) reported in Nyiragongo and Karisimbi health zones. Source: line list of Nyiragongo and Karisimbi Health Zones.
In Nyiragongo, the number of new cholera cases (suspected and confirmed) increased from 51 in week 47 (21-27 November) to 556 cases in week 50 (12-18 December) of the year 2022, and to 683 cases in week 52 (December 26, 2022-January 1, 2023).
On 14 December 2022, a cholera epidemic was officially declared by the Governor of the province of North Kivu, following isolation of Vibrio cholerae in the stool of 140 cases from Nyiragongo HZ at the local laboratory in Goma.
As of 4 February 2023, a total of 4386 cholera cases (1009 laboratory-confirmed; 23%) with 16 deaths (CFR 0.4%) have been reported, of which 4011 (91.5%) are from Nyiragongo and 375 (8.5%) from Karisimbi. In the HZ of Nyiragongo, the most affected age group is 5-14 years (30.1%), followed by 1-4 years (29.7%) and 15 -29 years (16.6%); children under the age of one represent 8% of cases.
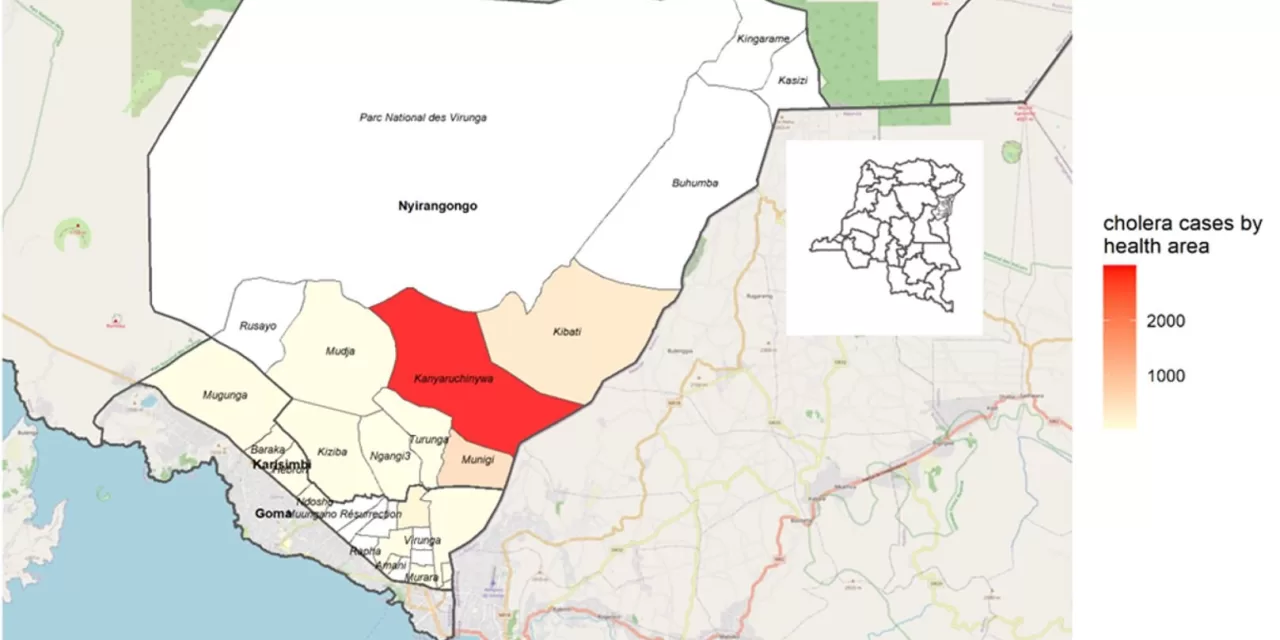
In total, 15 health areas including seven in the Nyiragongo HZ (Kanyaruchinya, Kibati, Kiziba, Mudja, Munigi, Ngangi III and Turunga) and eight in Karisimbi HZ (Baraka, Bujovu, Kasika, Katoyi, Majengo, Methodiste Mugunga and Muugano Solidarite) are currently affected by the cholera epidemic.
In the HZ of Nyiragongo, the health area of Kanyaruchinya is the most affected, contributing to 73.3% of all suspected cholera cases reported from Nyiragongo. In Karisimbi HZ, the Methodist health area is the most affected with 59.4% of all cases, followed by Baraka and Lasika health areas (both contributing to 7.3% of cases from Karisimbi HZ).
Figure 2. Cumulative number of cholera cases (suspected and confirmed) by health area in Niyragongo and Karisimbi health zones, as of 4 February 2023. Source: Nord Kivu Provincial Health Division. 
The cholera outbreak is principally affecting internally displaced populations (IDPs), with 97% of the cases reported among IDPs in the HZ of Nyiragongo, and 59% of cases among IDPs reported from the Methodist health area of Karisimbi HZ, which houses the Don Bosco IDP camp.
However, the outbreak is also spreading across the surrounding communities with nearly 3% of the cases in the HZ of Nyiragongo and 41% of the cases in the HZ of Karisimbi belonging to the host community.
Epidemiology of cholera
Cholera is an acute enteric infection caused by ingesting the bacteria Vibrio cholerae present in contaminated water or food. It is mainly linked to insufficient access to safe drinking water and inadequate sanitation. It is an extremely virulent disease that can cause severe acute watery diarrhoea resulting in high morbidity and mortality, and can spread rapidly, depending on the frequency of exposure, the exposed population and the setting. Cholera affects both children and adults and can be fatal if untreated.
The incubation period is between 12 hours and five days after ingestion of contaminated food or water. Most people infected with V. cholerae do not develop any symptoms, although the bacteria are present in their faeces for 1-10 days after infection and are shed back into the environment, potentially infecting other people. The majority of people who develop symptoms have mild or moderate symptoms, while a minority develop acute watery diarrhoea and vomiting with severe dehydration. Cholera is an easily treatable disease. Most people can be treated successfully through prompt administration of oral rehydration solution (ORS).
The consequences of a humanitarian crisis – such as disruption of water and sanitation systems, or the displacement of populations towards inadequate and overcrowded camps – can increase the risk of cholera transmission, should the bacteria be present or introduced.
A multisectoral approach including a combination of surveillance, water, sanitation and hygiene (WASH), social mobilization, treatment, and oral cholera vaccines is essential to control cholera outbreaks and to reduce deaths.
Public health response
Coordination: multisectoral coordination has been established at the provincial level, and daily coordination meetings are held in Kaniyaruchinya (Nyiragongo HZ). The incident management system (IMS) was activated at the WHO office. A budgeted preparedness and response plan has been developed and several partners are involved in the response, including WHO, which supports the Provincial Health Division (PHD) in the implementation of the health sector response in collaboration with the Ministry of Health and the other partners, such as the United Nations High Commissioner for Refugees (UNHCR), International Organization for Migration (IOM), Médecins Sans Frontières (MSF), UNICEF, World Food Programme (WFP), and Save the Children.
Epidemiological surveillance and laboratory: a surveillance and laboratory commission has been set up by the North Kivu Provincial Health Division with the support of WHO and other partners. Four data managers have been trained and equipped with computers by WHO. Training on case definition has been provided to healthcare workers and community health workers (CHW); investigation teams have also been trained on active case finding. Surveillance activities are ongoing, including active case finding, alert notification and investigation, and contact tracing and follow-up. Data is collected daily from Oral Rehydration Points (ORP), Cholera Treatment Units (CTU) and Cholera Treatment Centers (CTC). Samples are regularly collected also from suspected cases registered outside the outbreak area in order to assess the extent of the epidemic. Data is analyzed on a daily basis and shared with partners for operational decision-making. WHO also supported the National Biological Research Institute in Goma with sample transportation.
Case management: WHO and partners supported the establishment of 56 ORPs in IDP sites, four CTUs (Kibati, Kanyarucinya, Kahembe, and Don Bosco) and two CTCs (Munigi, Kiziba) in the most affected health areas, with a total capacity of 205 beds. WHO and partners also provided support for the free provision of basic health care in functional health structures in the two affected health zones to ensure the maintenance of essential health services for vulnerable populations.
Infection Prevention and Control (IPC)/Water, Hygiene and Sanitation (WASH): an IPC/WASH commission has been set up by the North Kivu PHD and supported by partners including WHO and UNICEF. Systematic decontamination of households and public spaces is implemented by trained teams. Training for safe and dignified burials is also carried out. In IDP sites a total of 1706 latrines, 293 showers, 91 hand-washing stations and 62 well sites have been established. Regular supply of water is made through cisterns. Training for healthcare workers and hygiene workers on IPC practices is also carried out regularly.
Risk communication and community engagement: Several advocacy meetings were held with community leaders and political-administrative authorities. Community workers have been trained to raise awareness about cholera, and preventive measures are communicated door-to-door and during public meetings with the affected population.
Vaccination: At the national level, coordination meetings were organized to ensure the preparation of the vaccination campaign against cholera in the two affected health zones. WHO provided support to the Ministry of Health for the mobilization from the vaccination International Coordination Group (ICG) of 364 137 doses of oral cholera vaccines in the two affected HZs. With the support of The Global Alliance for Vaccines and Immunization (GAVI), after its launch by the Governor of North Kivu province on January 25, 2023, the Oral Cholera Vaccination (OCV) campaign in three HZs of North Kivu PHD (including in IDP sites) took place between 25-30 January 2023 and immunized 351 207 people aged one year and older out of a target of 364 137, i.e. partial coverage of 96.4%.
WHO risk assessment
Cholera is endemic in parts of DRC. In 2022, according to data from the National Integrated Disease Surveillance and Response System, a total of 18 403 suspected cases of cholera, including 302 deaths (CFR 1.6%), were notified in the DRC, in 104 HZs of 19 of the 26 provinces of the country.
However, the current epidemic is showing a rapid upsurge in a fragile context such as IDPs camps.
For years, DRC has been experiencing several armed and community conflicts, particularly in the east, putting the country in a state of unprecedented humanitarian and health crisis.
Due to internal armed clashes, which intensified in 2022, nearly 450 857 new IDPs arrived in North Kivu (which already hosts 1.9 million of IDPs). Of them, 53.4% (240 579) are hosted in the territory of Nyiragongo and particularly 97.7% (235 111) in IDPs sites, which are characterized by overcrowding, poor hygiene and sanitation conditions, very limited access to drinking water, latrines and basic health services. In addition, population movements are regularly observed between the affected HZs and the other HZs in the province of North Kivu as well as the rest of the country, where the populations also have limited access to drinking water, good hygiene and sanitation conditions, as well as to health care facilities.
Moreover, the current rainy season may favor the spread of the epidemic in other HZs.
With the ongoing armed conflicts, displacements are likely to continue, leading to a worsening of the humanitarian context and the vulnerabilities of the populations, including the need for basic social services. All this is evolving in a context of a fragile health system; recurrent attacks on hospital infrastructures and reduced availability of services. Other outbreaks are also ongoing (COVID-19, yellow fever, poliomyelitis, measles, mpox (monkeypox), meningitis, etc.) and there are extremely limited human, material and financial resources.
The risk of cholera spreading to neighboring countries cannot be ruled out. Indeed, there are population movements between the affected health zones and neighboring countries, including Rwanda and Uganda.
The affected HZs border the city of Goma, which has an international airport. Countries in the Great Lakes sub-region (Rwanda, Uganda, Burundi), which are most at risk of cholera importation from the current epidemic hotspots in North Kivu, have inadequate levels of access to health care, poor drinking water, hygienic and sanitary conditions. A cholera epidemic is also ongoing in Burundi with 120 suspected cases and 1 death reported as of 7 February 2023. This epidemic affects the city of Bujumbura, which is located on the shores of Lake Tanganyika on the border with South Kivu, with population movements across the border.
The outbreak is occurring against a backdrop of a surge in cholera outbreaks globally, which has constrained the availability of vaccines, tests, and treatments.
Considering the above-described scenario, WHO assesses the risk posed by this outbreak as high at the national and regional level, and low at the global level.
WHO advice
A multi-pronged approach is essential to combat cholera and reduce mortality. The measures used combine surveillance, improvement of water supply, sanitation and hygiene, social mobilization, treatment of the disease and oral cholera vaccines. Countries affected by cholera are advised to strengthen disease surveillance and national preparedness to rapidly detect and respond to possible outbreaks.
WHO recommends improving access to proper and timely case management of cholera cases, improving access to safe drinking water and sanitation infrastructure, as well as improving infection prevention and control in healthcare facilities. These measures along with the promotion of preventive hygiene practices and food safety in affected communities are the most effective means of controlling cholera. Effective risk communication and community engagement strategies are needed to encourage behavioral change and the adoption of appropriate preventive measures.
Measures aimed at improving environmental conditions include applying long-term sustainable solutions for water supply, sanitation and hygiene in cholera-prone areas. In addition to cholera, these interventions can also prevent a wide range of other water-borne diseases and contribute to achieving goals in education and the fight against poverty and malnutrition. Solutions for water supply, sanitation and hygiene related to cholera are in line with the Sustainable Development Goals.
Rapid access to treatment is essential during a cholera outbreak. Oral rehydration should be available in communities and not just in larger health centers that can offer intravenous infusions and management at any time. With rapid and appropriate care, the case fatality rate should remain below 1%.
Community mobilization must continue as an integral part of the response and should cover information on the symptoms of cholera, on the precautions to take to protect against the disease, and the need to promptly seek care when symptoms appear.
The OCV should be used in conjunction with improvements in water and sanitation to control cholera outbreaks and for prevention in targeted areas known to be at high risk for cholera.
WHO recommends Member States to strengthen and maintain surveillance for cholera, especially at the community level, for the early detection of suspected cases and to provide adequate treatment and prevent its spread. Early and adequate treatment limits the CFR of patients to less than 1%.
WHO does not recommend any travel or trade restrictions to the Democratic Republic of Congo based on the currently available information.
Further information
- World Health Organization (16 December 2022). Disease Outbreak News; Cholera – Global situation. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON426
- WHO. Cholera factsheets
- WHO. Working with communities to curb cholera in the Democratic Republic of the Congo
- ENDING CHOLERA, A GLOBAL ROADMAP TO 2030
- WHO. Outbreaks and Emergencies Bulletin, Week 4: 16 to 22 January 2023
- United Nations Office for the Coordination of Humanitarian Affairs (OCHA). DRC humanitarian highlights 1-31 January 2023.
Citable reference: World Health Organization (10 February 2023). Disease Outbreak News; Cholera – Democratic Republic of Congo. Available at https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON441