In recent years, laparoscopic cholecystectomy, the surgical removal of the gallbladder, has become a common treatment for patients diagnosed with gallstones. However, a new study highlights that this procedure may not always be necessary or effective for alleviating abdominal pain. Each year, around 100,000 people seek medical attention for abdominal pain, with approximately 30,000 being diagnosed with gallstones. Despite the rise in surgeries since the 1990s, international guidelines for when to perform this operation remain unclear.
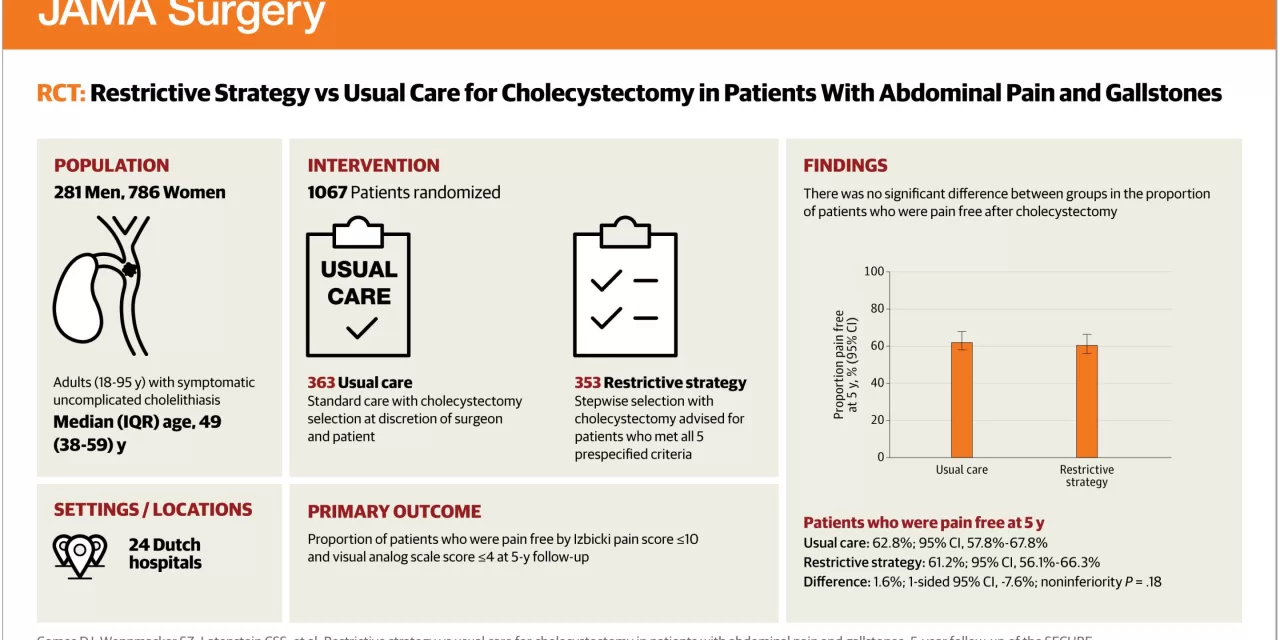
A study conducted by Radboud University Medical Center in 2019 investigated this issue by dividing patients with abdominal pain from gallstones into two groups. One group received the standard treatment of cholecystectomy, while the other was subjected to a restrictive selection strategy, where surgery was only considered after evaluating a range of pain symptoms. Though the number of surgeries decreased in the restrictive strategy group, about one-third of patients in both groups continued to experience abdominal pain a year later.
The study’s five-year follow-up, recently published in JAMA Surgery, reveals that the proportion of patients still experiencing pain remained unchanged: only two-thirds of patients were pain-free. Nevertheless, the restrictive strategy resulted in fewer unnecessary cholecystectomies without increasing complications related to gallstones or the surgery itself.
Dr. Daan Comes, the study’s lead author, emphasized the benefits of the restrictive approach. “We wanted to assess the long-term impact of a restrictive strategy on this patient population. Our findings suggest that while this approach is feasible and leads to fewer unnecessary surgeries, it is crucial to select the right patients for this strategy.”
In 2021, Radboudumc developed a decision rule to improve patient selection for surgery. Dr. Philip de Reuver, surgeon and principal investigator, noted, “Intense, episodic pain strongly indicates the need for surgery. However, patients with symptoms such as bloating, heartburn, or persistent pain might not benefit from cholecystectomy and should be evaluated for other conditions first.”
De Reuver is now initiating a follow-up study on the effectiveness of lifestyle interventions for patients whose symptoms suggest limited benefit from surgery. He believes that such interventions could enhance patient health and quality of life while potentially reducing the need for surgery.
“The goal is to reduce the daily number of gallbladder surgeries in the Netherlands, which currently stands at around 65. By doing so, we can save resources and improve patient outcomes,” De Reuver concluded.
For more details, refer to the study “Restrictive Strategy vs Usual Care for Cholecystectomy in Patients With Abdominal Pain and Gallstones” published in JAMA Surgery (2024).