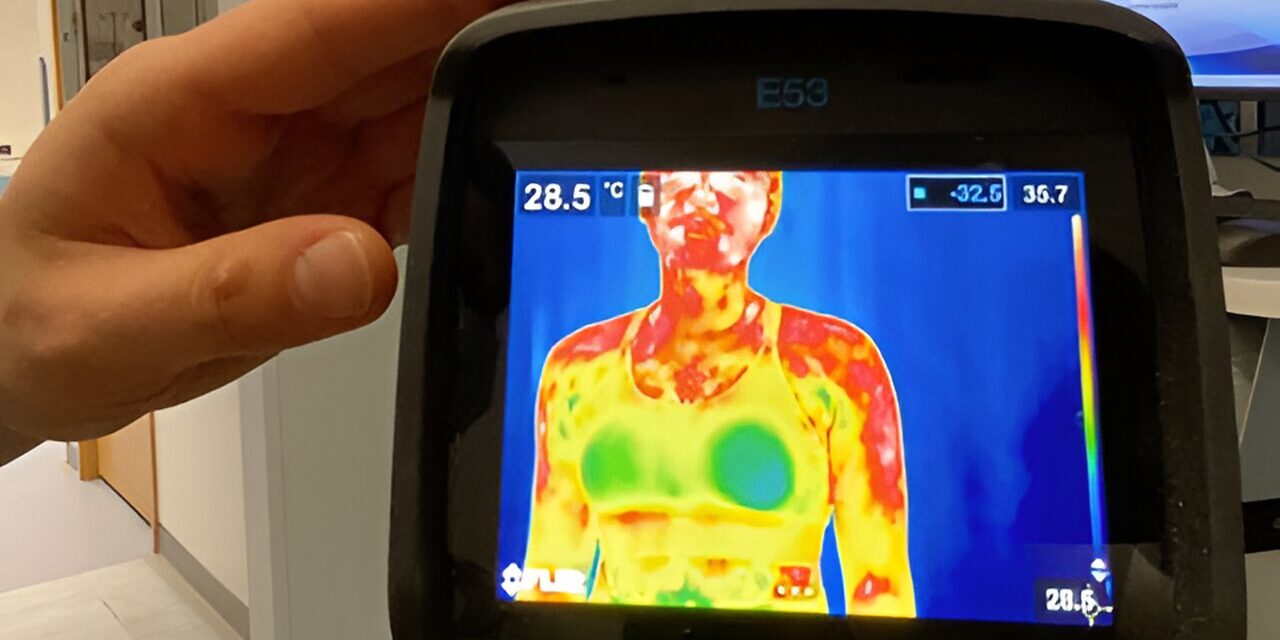
A recent study published in Plastic and Reconstructive Surgery suggests that breast-conserving therapy (BCT) offers better sexual well-being outcomes for women with breast cancer compared to mastectomy followed by breast reconstruction. The research, led by Dr. Jonas A. Nelson of Memorial Sloan Kettering Cancer Center, highlights the importance of addressing sexual health concerns when discussing breast cancer treatment options.
Key Findings from the Study
The study analyzed data from 15,857 breast cancer patients who underwent surgery between 2010 and 2022. Among them, 54% underwent BCT—also known as lumpectomy—while 46% had postmastectomy breast reconstruction (PMBR). Using the BREAST-Q questionnaire, researchers assessed sexual well-being, including factors such as sexual attractiveness, confidence, and comfort during intimacy.
Before surgery, both groups had similar average sexual well-being scores (62 for BCT and 59 for PBMR on a 0-to-100 scale). However, six months post-surgery, the BCT group’s score improved to 66 and remained stable over five years, whereas the PBMR group had lower scores, averaging 49 at six months and only improving to 53 over time. Notably, patients who had not yet completed their reconstruction had an even lower average score of 41.
Overall, the study found that patients undergoing BCT had an average sexual well-being score that was 7.6 points higher than those who had PMBR. This suggests that BCT may offer a superior choice for women concerned about maintaining their sexual well-being post-treatment.
Limited Access to Sexual Medicine Consultation
Despite the significant impact of breast cancer treatments on sexual health, only a small percentage of patients received sexual medicine consultations—3.5% in the BCT group and 5.4% in the PBMR group. The study noted that PMBR patients were about half as likely to receive these consultations compared to BCT patients, underscoring a gap in post-treatment care.
Implications for Breast Cancer Patients and Healthcare Providers
The findings reinforce previous research indicating that women who opt for BCT recover their sexual well-being more quickly than those undergoing PMBR. Dr. Nelson and his colleagues emphasize the importance of discussing sexual well-being as part of breast cancer treatment planning.
“Although many patients experience challenges in sexual health after breast cancer treatment, most do not receive specialized medical guidance,” said Dr. Nelson. “This presents an opportunity for healthcare providers to enhance post-treatment care by addressing sexual well-being concerns.”
Conclusion
For women eligible for both BCT and mastectomy, BCT may be a preferable option in terms of maintaining sexual well-being. The study underscores the need for greater awareness and access to sexual health support services for breast cancer patients.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. Patients are encouraged to consult their healthcare providers to discuss their specific treatment options and concerns regarding sexual well-being.