In a groundbreaking development poised to transform the landscape of heart transplantation, researchers have achieved a major breakthrough by successfully preserving transplanted pig hearts outside the body for over 24 hours. This remarkable feat, accomplished through a process called normothermic ex-vivo heart perfusion (NEHP), could revolutionize the field of transplantation by significantly extending the window for heart preservation beyond the current six-hour limit.
Published in the esteemed journal Frontiers in Cardiovascular Medicine, the study conducted by researchers at the University of Michigan Medical School at Ann Arbor marks a significant advancement in overcoming the critical bottleneck of heart availability for transplantation. With over 5,000 hearts transplanted annually worldwide, the demand far exceeds the supply, leaving up to 50,000 individuals in need of a heart at any given time.
Lead researcher Dr. Robert Bartlett, an emeritus professor and head of the Extracorporeal Life Support Laboratory, described the groundbreaking achievement as a potential game-changer in the field of transplantation. By utilizing NEHP, hearts removed from donors can be kept in a partly physiological state at room temperature, allowing for extended preservation and enhancing the viability of donor hearts for transplantation.
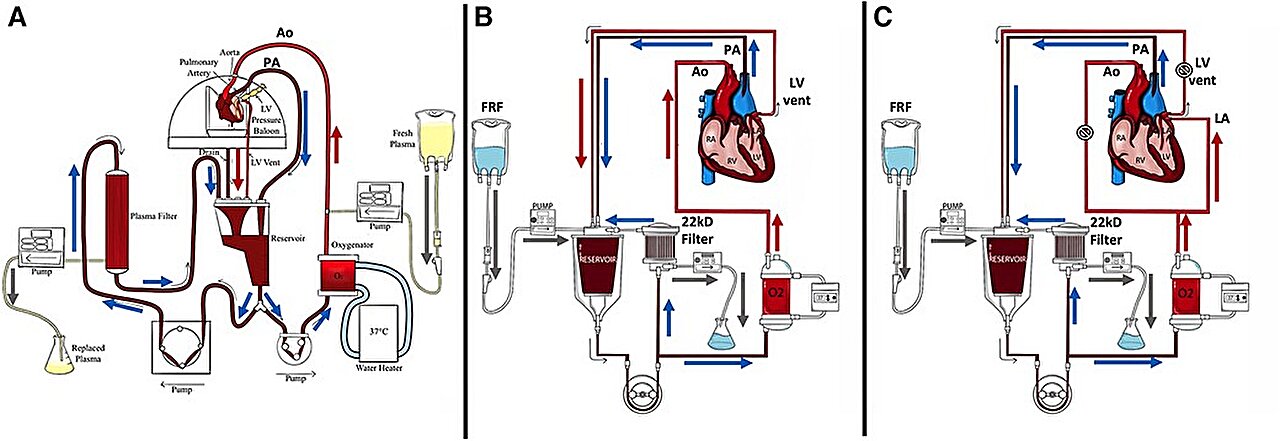
The NEHP process involves pumping oxygenated, nutrient-rich fluid through the hearts, facilitating the delivery of drugs and tissue-repairing stem cells. Through meticulous experimentation, the researchers refined NEHP variants, including hemofiltration and plasma exchange, to enhance heart preservation.
In a series of experiments involving immature and juvenile pig hearts, the researchers demonstrated the effectiveness of NEHP variants in maintaining heart viability for extended periods. Notably, hearts preserved with modifications to standard NEHP protocols survived for the full 24-hour duration, showcasing the potential of these advancements in revolutionizing heart transplantation.
Dr. Bartlett emphasized the transformative implications of this breakthrough, envisioning a future where the extended preservation of donor hearts could significantly increase the donor pool and improve outcomes for transplantation candidates. By providing an objective assessment of donor heart viability, these advancements could reduce the number of hearts that go unused due to uncertainty about their function.
Dr. Alvaro Rojas-Pena, a research investigator at the institute and corresponding author of the study, highlighted the next steps in translating these findings to clinical practice. The researchers are working towards validating the methods in humans, collaborating with human hearts rejected for transplantation to pave the way for real-world applications.
The study’s findings offer a beacon of hope for individuals awaiting life-saving heart transplants and underscore the transformative potential of innovative approaches in transplantation research. As researchers continue to push the boundaries of possibility, the future of heart transplantation appears increasingly promising, with the potential to save countless lives and alleviate the burden of heart disease worldwide.