A groundbreaking study has shed light on the perplexing visual distortions experienced by individuals grappling with a rare visual disorder known as prosopometamorphopsia (PMO), offering crucial insights into its accurate depiction and potential misdiagnosis.
For more than two years, a 58-year-old man has been haunted by haunting visual encounters, perceiving “demonic”-looking human faces whenever he interacts with others. These eerie distortions, characteristic of PMO, have long confounded medical professionals, often leading to misdiagnoses and inappropriate treatments akin to mental illness.
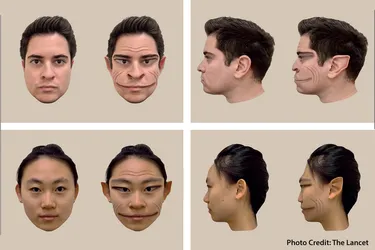
In a landmark research endeavor, experts from Dartmouth College harnessed computer software to craft faithful representations of the facial distortions perceived by PMO patients. By collaborating closely with a patient afflicted by the disorder, the team unraveled the intricate nuances of PMO, which manifest as warped perceptions of facial shape, texture, position, or color.
Dr. Brad Duchaine, Professor in the Department of Psychological and Brain Sciences at Dartmouth College, underscored the significance of the study’s findings in elucidating the severity of facial distortions experienced by PMO patients. “A substantial number of people we have worked with have been misdiagnosed, often with schizophrenia or some sort of psychotic episode,” Dr. Duchaine remarked, emphasizing the critical need for accurate diagnosis and tailored interventions.
Despite PMO’s rarity, believed to be underestimated given its misdiagnosis prevalence, the disorder’s underlying mechanisms remain elusive. While neurological events or structural brain changes may precipitate PMO, its onset can occur without discernible triggers, adding to its enigmatic nature.
The study’s patient, who endured a significant head injury and carbon monoxide exposure prior to symptom onset, exemplifies the multifaceted nature of PMO etiology. Notably, the patient’s distortions were influenced by color, with red intensifying distortions and green mitigating them, prompting the adoption of green-filtered glasses to alleviate symptoms in specific scenarios.
By leveraging real-time feedback and photo-editing software, researchers achieved a remarkable feat: visualizing the patient’s distorted perceptions in a tangible form, a pivotal step in validating the realities of PMO experiences. Dr. Duchaine expressed optimism that such insights would dispel misconceptions surrounding PMO, urging clinicians to approach visual distortions with heightened awareness and precision.
As medical science unravels the mysteries of rare disorders like PMO, each revelation brings us closer to personalized treatments and enhanced patient care. With further research and collaboration, the journey to unraveling PMO’s complexities promises to pave the way for transformative breakthroughs in visual healthcare.