“It is time to stop decades of failure. We have a lot to do to #EndTB by 2030,” said Professor (Dr) Guy Marks, President of the International Union Against TB and Lung Disease (The Union), at the opening of the largest TB and lung health conference this year in Bali, Indonesia (Union World Lung Health Conference 2024).
Marks is bang on spot. Historically, we never ever have been on track to end TB in high TB burden countries. At best we have been diagnosing and treating TB and saving lives – and preventing some of TB – but majorly failing to arrest the infection-spread and end TB. If we could prevent TB, then how come 10.8 million people got infected with TB last year as per the new WHO Global TB Report 2024? This amounts to TB prevention failure 10.8 million times last year itself.
Of course, over the decades a lot of work has been done to control TB– but we are still not in TB elimination mode. Millions have got lifesaving TB services but millions more have also got newly infected with TB – year after year. Millions of lives have been saved of TB but over a million die of TB – year after year. We need to face these inconvenient truths that reflect decades of failure – and truly and fully transition from TB control to #endTB response.
Primarily, with an array of evidence-based tools to prevent TB, no one should get infected with TB in the first place – or die of it. Even one TB death is a death too many.
TB treatment is also prevention, because soon after a person with TB disease gets on an effective treatment, infection stops spreading. Nutrition, tobacco control, alcohol control, HIV and diabetes prevention and management, optimal infection control, are important ways to reduce the risk of TB.
If we can find all TB early enough (when it is asymptomatic) and accurately, and link each of the persons diagnosed to effective TB treatment, and support them fully through their treatment and care, we can help shift gears from TB control mode to TB elimination mode.
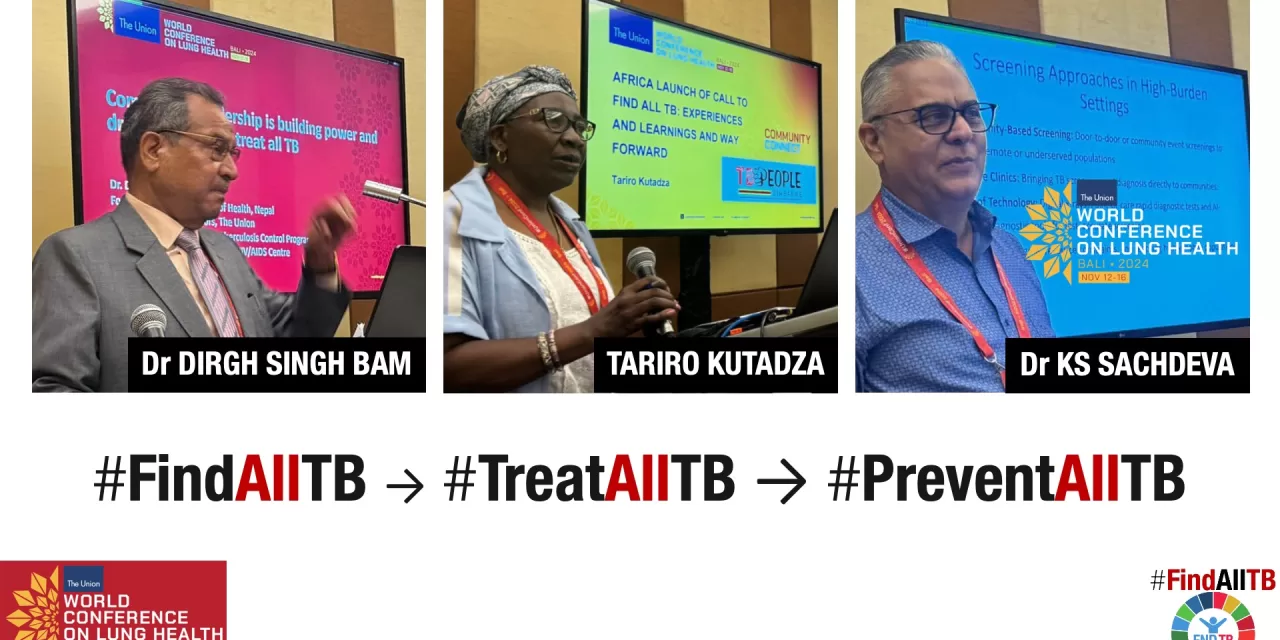
Legend speaks: Dr Dirgh Singh Bam at WCLH 2024
“TB despite being curable, killed over a million people each year and affected millions more,” said Dr Dirgh Singh Bam, who was delivering his opening keynote address at a session of the global meet. Dr Bam is a noted chest physician, and a former Health Secretary of Government of Nepal; former Director of National TB Programme, Ministry of Health and Population, Nepal; former Director of SAARC TB Centre; and former member of Board of Directors, The Union.
“TB has deeply rooted in several communities around the world as a health crisis, social and economical burden. All stakeholders including TB survivors have to collaborate effectively to find all people with TB – early and accurately – and treat all of them. Community leadership is a force for change when it comes to ensuring equitable access to full cascade of TB, health and social services for everyone – especially those likely to be left behind,” said Dr Bam. He called for stronger political commitment at all levels – including sub-national level so that well-coordinated local actions can deliver on the promises enshrined in global goals.
Screen everyone regardless of TB symptoms in high burden settings
While speaking in a WCLH 2024 session on finding, treating and preventing all TB, Dr Kuldeep Singh Sachdeva, reiterated that to eliminate TB we must try to screen the entire population for TB, offer upfront WHO recommended molecular testing to all those with presumptive TB, and put them on treatment without delay. Dr Sachdeva served an illustrious tenure earlier as head of Indian government’s TB and HIV programmes, and also served as Southeast Asian Director of The Union. Currently, he leads Molbio Diagnostics as President and Chief Medical Officer.
“We must also look for TB in the not-so-vulnerable populations. You will find 50% of TB in non-vulnerable and non-symptomatic populations. It has been demonstrated in various surveys that 50-60% of individuals who test positive for TB do not have any symptoms and look healthy – they will have symptoms 6 months later when the disease has advanced [and has spread to many more]. Aim of eliminating TB is to find them as early as possible. You can find 50% of the estimated TB in healthy population, if you reach them through the existing tools of TB screening,” he said.
Thanks to science, today we have the tools to find all TB, treat all TB and prevent all TB, (and stop the spread of infection) even for those living in disadvantaged and/or difficult to reach areas. We have WHO recommended ultraportable handheld and battery-operated x-ray machines to screen people for TB; we have WHO approved point of care, battery-operated, molecular diagnostic tools like Truenat; we have shorter and patient-friendly treatment regimens that can effectively cure drug-sensitive and drug-resistant TB; and we have TB preventive treatment to prevent TB along with science-backed ways to prevent TB (such as infection control, tobacco and alcohol control, nutrition, NCDs and HIV prevention and control, among others).
But unless we deploy these tools on the ground to find the so called ‘missing TB cases’ and put them on treatment and care we will never be able to eliminate TB.
Unacceptable: Missing TB among those who take a TB test
Finding all TB early and accurately needs the programme to be rooted in elimination mode. But quite a number of public health programmes are not even geared to find all TB in people who come to health facilities for TB diagnosis, forget about the “missing TB cases.”
Way back in 2018, WHO had asked governments to replace the underperforming microscopy test with 100% upfront molecular testing by 2027. World leaders also re-echoed this goal at the United Nations General Assembly High-Level Meeting on TB in 2023.
Yet, as per the WHO Global TB Report 2024 less than 50% of the new TB cases in 2023 could get upfront molecular testing globally- the rest got microscopy that is an outdated test and misses 50% of the cases. So, we missed the other half of people who had TB and took a TB test – we missed them because we used a bad test. The situation is more dismal in South-East Asia where less than 40% could access molecular testing in 2023. In Africa, 54% of TB patients could get diagnosed on a molecular test.
As per India TB Report 2024, TB case notifications increased to 179 cases per 0.1 million population in 2023 (2.55 million TB cases were notified). However, only 21% of the presumptive TB cases were offered a rapid molecular diagnostic test.
Presumptive TB testing by microscopy increased by 40% (from 986.6 per 0.1 million population in 2022 to 1352 per 0.1 million population in 2023). This totally overshadows the 22% increase in rapid molecular testing for the same period.
End inequities and injustices that plague the TB response
Till we get a safe and effective TB vaccine, let us at least rollout the currently existing TB tools that are available for diagnostics, treatments, and prevention – equitably – and chart a pathway to help rollout other upcoming new technologies with equity and justice in future. We cannot be paralysed with a dream of a futuristic vaccine, when we are failing miserably to rollout best of health technologies with equity and justice today.
“Racial inequity and injustices, as well as lack of political will and commitment, continue to plague the TB response. Majority of the TB burden is in poor – low- and middle-income countries in the Global South where most of new TB infections as well as TB deaths occur. Recently a public health emergency was declared in Long Island USA, when one TB case was reported. Dozens of contact tracings were done. But in many countries of the Global South, TB is a public health emergency, and a social justice emergency every single day,” rightly said Tariro Kutadza, firebrand health justice and human rights activist who leads TB People (Zimbabwe). TB People (Zimbabwe) had launched the Africa call to find all TB at largest AIDS and STIs conference in Africa in 2023 (ICASA).
“We can end TB now if we end inequity and social injustices. We can end TB if we deploy the best of existing TB diagnostic, treatment and prevention services in a people-centric, gender transformative and rights-based manner– with standard WHO recommended screening and upfront diagnostic tools. Ending inaccurate and delayed diagnosis of TB will help reduce catastrophic costs too and break the chain of infection transmission,” added Kutadza.
TB programmes will have to screen everyone (and not just those with TB symptoms) with WHO recommended screening tools; confirm those with presumptive TB using molecular tests; put them on appropriate treatment and ensure that they complete the treatment in a socially just and equitable manner.
Global call to find all TB to stop TB
The Global Call to Find All TB to Stop TB was launched in 2023 by organisations and individuals who united to find all TB in people-centred and rights-based manner – and link all of them to care: www.bit.ly/findalltb . It has been endorsed by over 2000 organisations and individuals so far including The Union.
The call has the key ask to stop missing TB cases, and 2 action points:
1) 100% replacement of sputum smear microscopy with WHO recommended molecular tests as soon as possible, along with a shift from a lab-centric to a people-centric model to find TB, leaving no one behind.
2) Find the missing millions by screening everyone (and not just those with TB symptoms) with WHO recommended screening tools and confirm those with presumptive TB using molecular tests.
Let us hope we are able to end TB and advance progress towards all other goals and targets enshrined in SDGs for 2030. Only 73 months are left and urgency to get on the right track to end TB and deliver on all SDGs is not only compelling but also a human rights imperative.
Shobha Shukla – CNS (Citizen News Service)