In a groundbreaking study led by researchers from University College London (UCL), artificial intelligence (AI) has shed light on a gender disparity in diagnosing hypertrophic cardiomyopathy (HCM), a potentially life-threatening heart condition. The findings, published in the Journal of the American College of Cardiology, could revolutionize diagnostic guidelines, ensuring more equitable and accurate identification of the disease.
The Diagnosis Gap
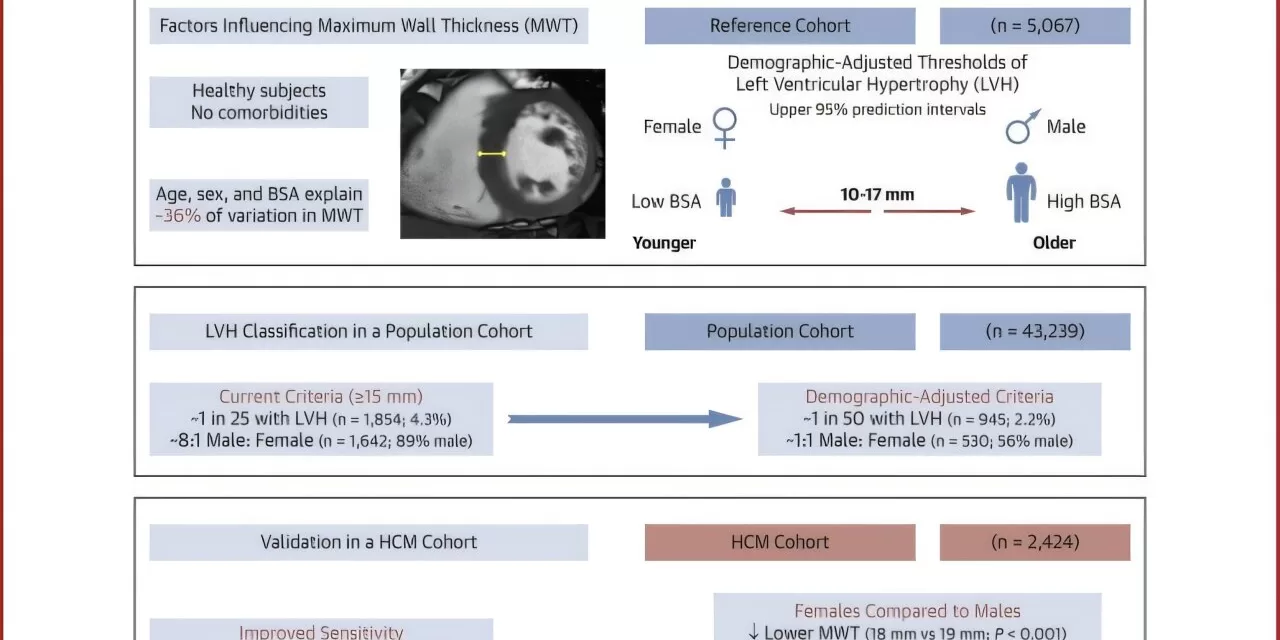
HCM, a genetic condition affecting about one in 500 people in the UK, thickens the heart’s muscular wall, impairing its ability to pump blood effectively. While the condition is known to impact men and women equally, current diagnostic practices have disproportionately identified men, with two-thirds of diagnosed cases attributed to them.
The traditional diagnostic benchmark—a 15-millimeter threshold for heart muscle thickness—has remained unchanged for over 50 years. However, this one-size-fits-all standard fails to account for individual differences in sex, age, and body size, potentially leaving many women undiagnosed.
Personalized Approach Boosts Diagnosis
The UCL research team, led by Dr. Hunain Shiwani, developed an AI-powered tool capable of analyzing MRI heart scans with unmatched precision. Using data from 5,000 scans of healthy hearts, the AI defined “normal” heart wall thickness across various demographics. This enabled the researchers to establish personalized diagnostic thresholds that adjust for factors such as age, sex, and body surface area.
Testing their updated approach on 1,600 patients with confirmed HCM revealed a striking improvement: diagnosis rates for women increased by 20 percentage points. Applying these personalized thresholds to a larger sample of 43,000 individuals from the UK Biobank further highlighted its efficacy. Unlike the current method, which identified only one woman for every eight diagnoses, the new approach achieved a near-equal gender distribution, with women comprising 44% of identified cases.
Implications for Patients and Clinicians
The study emphasizes the critical need for personalized medicine. “Having the same cut-off for everyone completely ignores the fact that heart wall thickness is strongly influenced by age, sex, and size,” said Dr. Shiwani. “Effective treatments for HCM are starting to emerge, making it more important than ever to correctly identify those who need them.”
By refining diagnostic criteria, the updated method not only identifies more women but also reduces false positives. This means fewer people endure the psychological and medical burdens of a misdiagnosis, ensuring treatments are directed to those who genuinely need them.
Future Prospects
To further enhance the diagnostic process, the research team plans to incorporate additional factors like ethnicity and adapt their thresholds for use with echocardiograms—more commonly available in clinical settings. They aim to establish updated guidelines across Europe and America, making personalized diagnostics a standard practice.
Dr. Sonya Babu-Narayan, Clinical Director at the British Heart Foundation, hailed the research as a “new era” for HCM diagnosis. “This more personalized approach ensures that individuals—especially women and those of smaller stature—are no longer overlooked, offering hope for improved outcomes.”
A Paradigm Shift
The study exemplifies the transformative potential of AI in healthcare, not only addressing gender disparities but also enhancing overall diagnostic accuracy. With further refinements, this approach could redefine how HCM and similar conditions are identified, ensuring that patients receive timely and effective care.
Reference:
Hunain Shiwani et al., Demographic-Based Personalized Left Ventricular Hypertrophy Thresholds for Hypertrophic Cardiomyopathy Diagnosis, Journal of the American College of Cardiology (2025). DOI: 10.1016/j.jacc.2024.10.082