Millions of Americans undergo surgery each year, and preventing postoperative complications such as pneumonia, blood clots, and infections can mean the difference between a successful recovery and a prolonged hospital stay—or worse. More than 10% of surgical patients experience complications, leading to longer intensive care unit (ICU) stays, higher mortality rates, and increased healthcare costs. Early identification of at-risk patients is crucial, yet accurate risk prediction remains a challenge.
A breakthrough in artificial intelligence (AI), particularly large language models (LLMs), is now offering a promising solution. A recent study led by Chenyang Lu, the Fullgraf Professor in Computer Science & Engineering at the McKelvey School of Engineering and Director of the AI for Health Institute (AIHealth) at Washington University in St. Louis, demonstrates that specialized LLMs can significantly outperform traditional machine learning methods in forecasting postoperative risks. The research, published in npj Digital Medicine, highlights the transformative potential of AI in surgical care.
Harnessing AI for Better Predictions
“Surgery carries significant risks and costs, yet clinical notes hold a wealth of valuable insights from the surgical team,” Lu stated. “Our large language model, tailored specifically for surgical notes, enables early and accurate prediction of postoperative complications. By identifying risks proactively, clinicians can intervene sooner, improving patient safety and outcomes.”
Traditional risk prediction models rely primarily on structured data, such as laboratory results, patient demographics, and surgical details. While these factors are valuable, they often lack the nuance captured in a patient’s clinical narrative. Detailed surgical notes provide personalized accounts of a patient’s medical history and current condition—critical elements that influence the likelihood of complications.
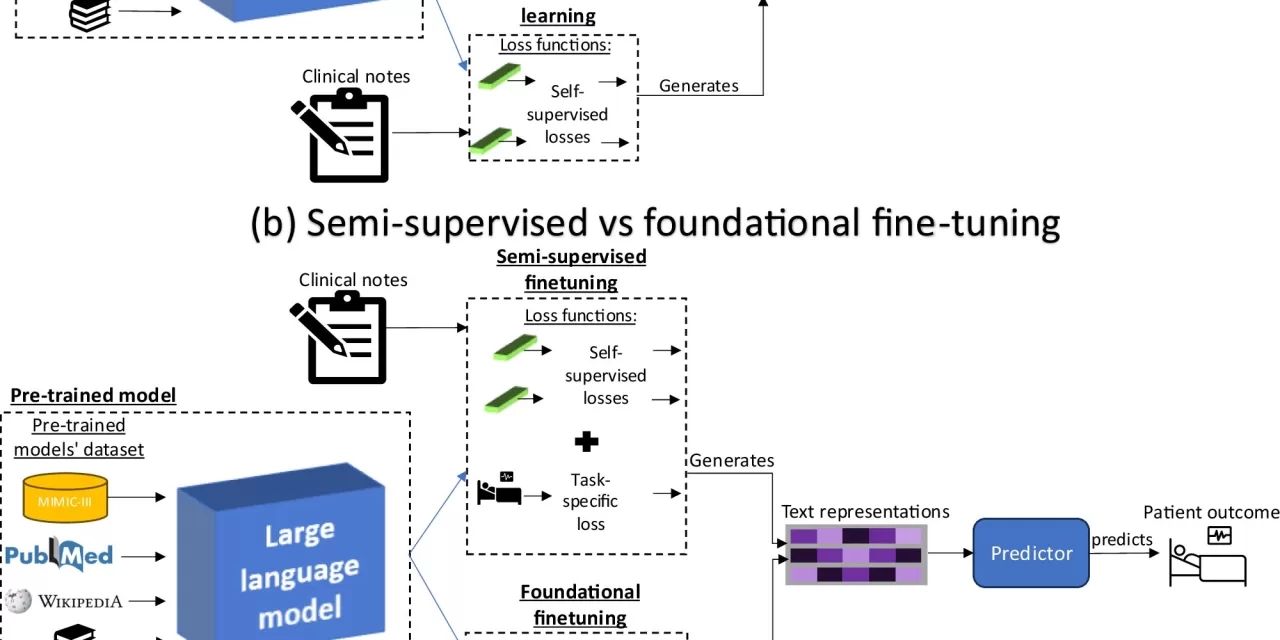
Lu and co-first authors Charles Alba and Bing Xue, both graduate students at Washington University at the time of the study, trained specialized LLMs on publicly available medical literature and electronic health records. The team fine-tuned these pretrained models on surgical notes, enabling them to detect patterns in patient conditions that might otherwise be overlooked. This innovative method—the first of its kind—demonstrates that analyzing textual clinical data can dramatically improve risk predictions.
Strong Performance in Real-World Data
The model was tested on nearly 85,000 surgical notes and associated patient outcomes collected from an academic medical center in the Midwest between 2018 and 2021. Results showed that the AI system significantly outperformed traditional methods. Specifically, for every 100 patients who experienced a postoperative complication, the new AI model correctly predicted 39 more cases compared to previous natural language processing models.
Beyond improving individual patient outcomes, the study also highlights the power of foundational AI models, which can be adapted for multiple medical tasks. “Foundation models can be diversified, so they’re generally more useful than specialized models. In this case, where lots of complications are possible, the model needs to be versatile enough to predict many different outcomes,” said Alba, a graduate student in WashU’s Division of Computational & Data Sciences.
“We fine-tuned our model for multiple tasks simultaneously and found that it predicts complications more accurately than models trained for individual complications,” Alba added. “This makes sense because complications are often correlated, so a unified foundational model benefits from shared knowledge about different outcomes and doesn’t have to be painstakingly tuned for each one.”
Future Implications for Healthcare
Joanna Abraham, Associate Professor of Anesthesiology at WashU Medicine and a member of the Institute for Informatics (I2) at WashU Medicine, emphasized the model’s real-world potential. “This versatile model has the potential to be deployed across various clinical settings to predict a wide range of complications. By identifying risks early, it could become an invaluable tool for clinicians, enabling them to take proactive measures and tailor interventions to improve patient outcomes.”
As AI continues to revolutionize healthcare, advancements like this suggest a future where predictive models help clinicians make more informed decisions, ultimately improving surgical outcomes and reducing healthcare burdens.
More Information: Charles Alba et al, The foundational capabilities of large language models in predicting postoperative risks using clinical notes, npj Digital Medicine (2025). DOI: 10.1038/s41746-025-01489-2
Disclaimer: This article is based on academic research and does not constitute medical advice. AI models are tools to assist clinicians, and their predictions should be used in conjunction with expert medical judgment. Further validation in real-world clinical settings is required before widespread adoption.