A groundbreaking artificial intelligence (AI) model has been developed to identify female patients at a higher risk of heart disease using electrocardiograms (ECGs). Researchers believe this AI-driven approach could enable earlier detection and better treatment for women who may otherwise be overlooked. The findings were published in The Lancet Digital Health.
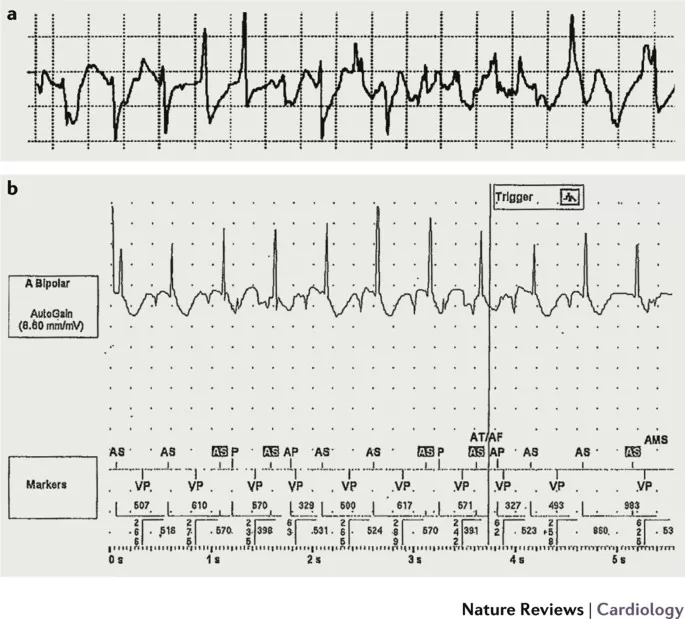
An ECG is a widely used test that records the electrical activity of the heart. In this study, researchers applied AI to analyze over one million ECGs from 180,000 patients, including 98,000 women. The AI model assigns a score to ECGs, assessing how closely an individual’s results align with typical male or female patterns.
Women whose ECGs resembled typical male patterns—such as exhibiting larger electrical signals—were found to have larger heart chambers and greater muscle mass. Importantly, these women also showed a significantly increased risk of cardiovascular disease, heart failure, and heart attacks when compared to those with ECGs more typical of female heart patterns.
Historically, cardiovascular disease has been perceived as a predominantly male health issue. While men do tend to have a higher risk of heart disease due to hormonal and lifestyle differences, cardiovascular disease remains the leading cause of death among women. In the UK, women are twice as likely to die from coronary heart disease—the leading cause of heart attacks—than from breast cancer.
A recent consensus statement highlighted cardiovascular disease as the “number one killer” of women and called for improvements in diagnosis, treatment, and female representation in clinical research.
Dr. Arunashis Sau, an Academic Clinical Lecturer at Imperial College London’s National Heart and Lung Institute and a cardiology registrar at Imperial College Healthcare NHS Trust, led the study. He emphasized the complexity of cardiovascular disease in women, stating: “Our work has underlined that cardiovascular disease in females is far more complex than previously thought. The AI-enhanced ECGs give us a more nuanced understanding of female heart health—and we believe this could be used to improve outcomes for women at risk of heart disease.”
Dr. Fu Siong Ng, a Reader in Cardiac Electrophysiology at Imperial College London and consultant cardiologist, co-authored the study. He pointed out that many women flagged by the AI were actually at greater risk than the average man. “If widely implemented, this AI model could reduce gender disparities in cardiac care and improve outcomes for women at risk of heart disease,” he added.
The research team previously developed an AI-ECG risk estimation model called AIRE, which predicts a patient’s likelihood of developing heart disease based on ECG data. Trials of AIRE in the UK’s National Health Service (NHS) are planned for late 2025, aiming to assess its benefits in real-world clinical settings across multiple hospitals.
Dr. Sonya Babu-Narayan, Clinical Director at the British Heart Foundation, reinforced the importance of such research. “Far too often, women are misdiagnosed or even dismissed by health care professionals due to the misconception that heart disease primarily affects men. This study demonstrates how AI could enhance ECG interpretation, helping identify women at the highest risk of future heart problems. However, one test alone will not bridge the gender gap in heart care. Systemic change is necessary to ensure all patients receive appropriate and timely treatment.”
The potential of AI in cardiovascular care is promising, but researchers stress that further trials and clinical implementation will be key in translating these findings into real-world benefits for patients.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Patients should consult a healthcare professional for personalized diagnosis and treatment.