Stanford Medicine researchers have developed an AI-driven algorithm that utilizes continuous glucose monitor (CGM) data to identify distinct subtypes of type 2 diabetes, a breakthrough in precision medicine that could revolutionize diabetes care.
Type 2 diabetes, typically associated with obesity and adult onset, has traditionally been diagnosed based solely on blood glucose levels, grouping all patients into a broad category. However, recent research has revealed that this group is far from homogenous, with significant variability in factors such as age of onset, body weight, and underlying physiology. In response, scientists have increasingly focused on subclassifying type 2 diabetes to better address these differences and improve treatment outcomes.
A new study from Stanford Medicine, co-led by Dr. Michael Snyder, Professor of Genetics, introduces an AI-powered tool that uses data from widely accessible continuous glucose monitors (CGMs) to predict and identify three of the four most common subtypes of type 2 diabetes. These subtypes include insulin resistance, beta cell dysfunction, and other metabolic variations that can influence treatment choices.
“This tool could help individuals catch prediabetes early, offering them a chance to make preventative changes to their lifestyle, such as adjusting their diet or exercise habits,” said Dr. Snyder, a co-senior author of the study published in Nature Biomedical Engineering.
With approximately 40 million people in the U.S. diagnosed with diabetes, and another 98 million with prediabetes, the potential for such a tool to reshape diabetes care is immense. The ability to differentiate subtypes of type 2 diabetes could lead to more effective treatments, including personalized medication regimens and lifestyle interventions tailored to an individual’s specific metabolic profile.
Type 2 diabetes is typically associated with either insulin resistance, where the body’s cells fail to respond to insulin, or insulin deficiency, where the pancreas produces insufficient insulin. However, there are additional mechanisms that can contribute to the condition, including issues with incretin production or liver insulin resistance. Identifying the exact cause of elevated blood glucose levels is crucial, as treatments may vary depending on the subtype.
“We’re trying to make it easier for people to understand and improve their health,” said Dr. Tracey McLaughlin, a Professor of Endocrinology and co-senior author. “By subclassifying type 2 diabetes, we can offer more targeted therapies that have a higher chance of success.”
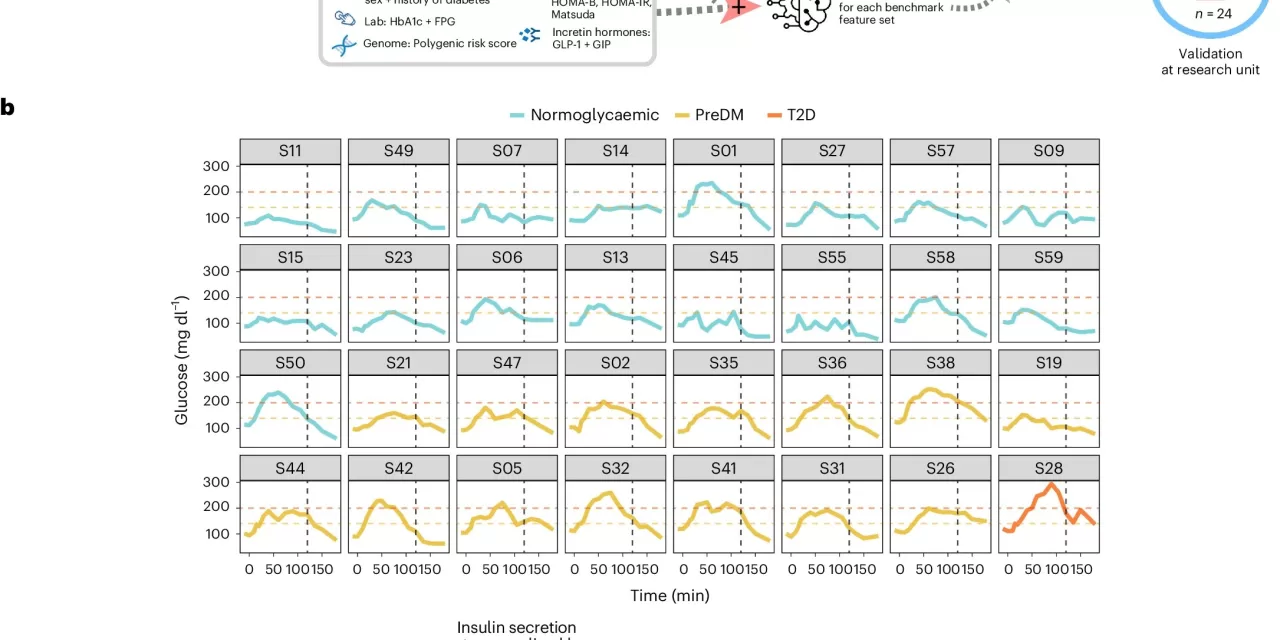
The AI algorithm leverages CGM data to analyze patterns in glucose fluctuations, which reveal underlying metabolic issues. When compared with traditional diagnostic tests, including the glucose tolerance test, the algorithm demonstrated a remarkable 90% accuracy rate in identifying subtypes of diabetes based on CGM data.
CGMs, which are worn on the arm, measure real-time fluctuations in blood glucose levels, providing a continuous, detailed picture of a person’s metabolic state. This technology not only offers greater accuracy than conventional diagnostic methods, but it also has the advantage of being accessible to people in the comfort of their own homes.
The study tested the algorithm on 54 participants, including individuals with prediabetes and healthy controls. The results revealed that the AI-powered analysis of CGM data could accurately predict metabolic subtypes, such as insulin resistance or beta-cell dysfunction, at home—offering a level of precision previously only achievable through invasive clinical testing.
The potential for this technology goes beyond diabetes management. For individuals with insulin resistance, even if they don’t progress to full-blown diabetes, knowing their status is crucial. Insulin resistance is a known risk factor for other serious conditions, including heart disease and fatty liver disease.
Looking ahead, McLaughlin and Snyder hope to expand the use of this algorithm, not only for those with prediabetes or type 2 diabetes but also as a tool for individuals who face challenges accessing healthcare. They believe that the widespread availability of CGMs and AI-driven diagnostics could provide critical support for underserved populations, particularly those in remote or economically disadvantaged areas.
“We see this technology as a way to provide access to high-quality care for people who might not otherwise be able to afford or reach a healthcare facility,” said Dr. McLaughlin.
This innovative approach represents a promising step forward in the fight against diabetes, offering individuals greater insight into their health while paving the way for more personalized and accessible care.
For further details on the study, you can read the full paper published in Nature Biomedical Engineering (DOI: 10.1038/s41551-024-01311-6).