New research supported by the National Institute for Health and Care Research (NIHR) has revealed that higher levels of inflammation in the blood of obese patients after undergoing bariatric surgery can lead to less successful weight loss outcomes six months post-surgery.
Conducted by scientists from King’s College London’s Institute of Psychiatry, Psychology & Neuroscience (IoPPN) and published in Psychological Medicine, this study is the first to investigate the link between depression and inflammation in obese individuals both before and after bariatric surgery. The findings suggest a significant correlation between depression and inflammation in obese patients before and after surgery, with elevated inflammation, rather than sadness, being identified as a key factor contributing to poor weight reduction results.
Lead author and Clinical Professor of Psychoneuroimmunology at IoPPN, King’s College London, Valeria Mondelli, highlighted the clinical implications of this study, emphasizing the identification of specific targets for personalized interventions that could enhance physical and mental health outcomes post-bariatric surgery. For example, the data showed that increased inflammation could predict lower weight loss after surgery, suggesting that tailored treatments focusing on inflammation reduction might improve post-surgery outcomes.
Obesity presents a substantial financial burden on the NHS, costing approximately £6 billion annually, with projections indicating an increase to £9.6 billion per year by 2050. Bariatric surgery, which involves physical modifications to the stomach and/or bowel to limit food intake and nutrient absorption, can lead to significant weight loss in obese patients, although results vary.
Understanding the factors influencing bariatric surgery outcomes is crucial to ensuring effective treatment for obesity, especially given the high costs involved in both public and private healthcare settings. Depression frequently co-occurs with obesity, and previous research has suggested that inflammatory proteins released as part of the immune response may be a shared mechanism driving both conditions.
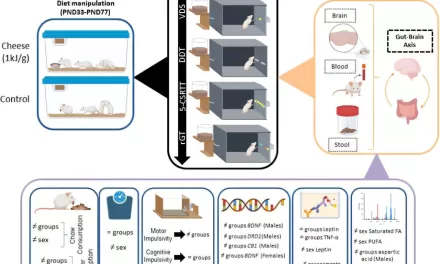
To delve deeper into this relationship and its implications for obesity and bariatric surgery outcomes, the study examined differences in inflammation-related protein levels between obese patients with and without depression who were undergoing surgery. The study involved 85 participants from King’s College Hospital NHS Foundation Trust in south London, all of whom had obesity (BMI > 35) and were part of the ongoing Bariatric Surgery & Depression study.
The researchers measured levels of inflammatory proteins, including C-reactive protein (CRP) and cytokines like interleukin-6 (IL-6) and interleukin-4 (IL-4), in participants’ blood and tissue before and after surgery. Before surgery, 41 participants exhibited symptoms of depression that met clinical diagnosis criteria, while the remaining 44 had subclinical depression symptoms.
The study found that individuals with depression had higher levels of inflammatory proteins CRP and IL-6 in their blood and lower levels of the anti-inflammatory protein IL-4. They also had elevated levels of a specific inflammatory protein in their adipose tissue. Six months post-surgery, patients who had depression before the procedure still had elevated levels of IL-6 and CRP in their blood, despite no significant difference in weight loss compared to those without depression.
Overall, bariatric surgery resulted in weight loss for all patients as expected, and most patients with pre-surgery depression experienced a reduction in their symptoms, no longer meeting clinical criteria for depression. Among the 44 patients with pre-surgery depression, 29 completed the six-month follow-up, and only about one-third (34.5%) of them still had clinical depression after surgery.
The researchers also explored whether inflammation and depression measures before surgery could predict weight loss and depression outcomes post-surgery. Their analysis revealed that higher CRP levels before surgery were associated with reduced weight loss at the six-month follow-up. However, depression levels before surgery and experiences of childhood trauma were more predictive of post-surgery depression than CRP levels before surgery.
Dr. Anna McLaughlin, the first author of the study and a Postdoctoral Research Associate at IoPPN, King’s College London, emphasized the significance of the findings. She noted that inflammation levels in the blood, rather than depression, played a crucial role in determining weight loss outcomes after bariatric surgery. Additionally, the research underscored the importance of providing psychological support to patients with a history of childhood trauma after surgery, as these factors influenced post-surgery depression outcomes. Integrating inflammation data with clinical insights will be vital for identifying risk factors and enhancing outcomes for bariatric surgery patients moving forward.