A new study from the University at Buffalo has found that exposure to air pollution during the final month of pregnancy significantly increases the risk of newborns requiring neonatal intensive care unit (NICU) admission. The study, published in Scientific Reports, highlights the impact of common air pollutants on fetal health, emphasizing the need for improved air quality measures.
The Role of Air Pollution
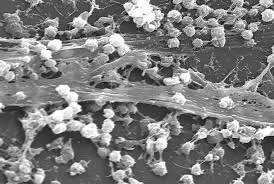
Air pollution from auto emissions, wildfires, and industrial processes has long been a health concern, but its effects on pregnant individuals and their babies remain a critical area of research. The study focused on pollutants such as nitrogen dioxide (NO2), which is primarily emitted by vehicles and industrial sources, and fine particulate matter (PM2.5), which consists of microscopic airborne particles. Researchers also examined ozone (O3), a secondary pollutant formed by chemical reactions in sunlight.
Key Findings
The researchers used satellite-based air pollution data to assess the effects of these pollutants on NICU admissions across the United States. Their analysis revealed that newborns exposed to higher levels of NO2 in the final month of pregnancy faced a 30–35% higher risk of NICU admission. Exposure to PM2.5 was linked to an 11–22% increased risk.
Dr. Yohane V.A. Phiri, the study’s lead author and a postdoctoral research associate at UB’s School of Public Health and Health Professions, stressed the significance of these findings.
“Our findings highlight the critical impact of air pollution during the final weeks of pregnancy, a time of heightened fetal vulnerability, and emphasize the significance of addressing air pollution exposure, even at lower levels,” Phiri stated.
Regional and Seasonal Differences
The study found regional and seasonal variations in risk. The Midwest and Mid-Atlantic regions had the highest odds of NICU admission linked to NO2 exposure, while PM2.5-related risks were most pronounced along the West Coast and Southeast, particularly during summer and winter months.
Interestingly, ozone exposure did not show a consistent increase in NICU admissions, and in some cases, it appeared to have a protective effect except during the summer.
Implications for Public Health
Despite advances in maternal and child healthcare, NICU admissions remain a concern in the U.S., with 8.1% of infants requiring intensive care in 2018, the year on which the study focused.
Phiri emphasized that while the findings do not establish direct causation, they support efforts to further reduce air pollution. “Such efforts could ultimately benefit pregnant women by minimizing exposure to harmful pollutants and reducing associated neonatal health risks,” he said.
The study, co-authored by researchers from the University of Maryland and the University of Massachusetts Amherst, used satellite-derived data to provide a comprehensive national analysis. This approach also enabled the inclusion of rural areas that may lack ground-based pollution monitoring.
Conclusion
The study underscores the urgent need to address air pollution exposure during late pregnancy, particularly in urban and industrial regions where pollution levels are higher. Public health initiatives aimed at reducing vehicle emissions and improving air quality standards could have a meaningful impact on maternal and infant health outcomes.
Disclaimer
The findings of this study do not establish a direct cause-and-effect relationship between air pollution exposure and NICU admissions. Further research is needed to explore additional contributing factors. Pregnant individuals concerned about air quality should consult healthcare professionals for guidance on minimizing exposure to pollutants.