Global overview Data as of 12 September 2021
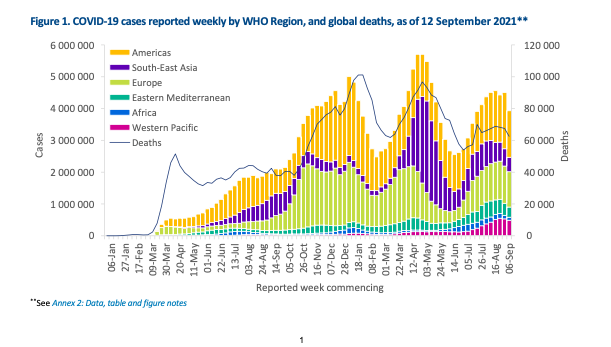
With nearly 4 million new cases reported globally in the past week (6-12 September), this represents the first substantial decline in weekly cases in more than two months (Figure 1). All regions reported declines in new cases as compared to the previous week.
The number of deaths reported globally in the past week also decreased as compared to the previous week, with just over 62 000 new deaths. The African Region reported an increase in the number of weekly deaths (7%), while the South-East Asia Region reported the largest decrease (20%). The American and Eastern Mediterranean Regions reported slightly smaller decreases, 9% and 6% respectively, while the numbers of deaths reported in the European and the Western Pacific Regions were similar to last week. The cumulative number of cases reported globally is now over 224 million and the cumulative number of deaths is just over 4.6 million.

The regions reporting the highest weekly incidence rates per 100 000 population of cases and of deaths remain the same as in the previous week: the Region of the Americas (143 new cases per 100 000 population; 2.3 deaths per 100 000 population) and European Region (119.4 new cases per 100 000 population; 1.5 deaths per 100 000 population).
The highest numbers of new cases were reported from the United States of America (1 034 836 new cases; 20% decrease), the United Kingdom (256 051 new cases; 5% increase), India (248 248 new cases; 15% decrease), the Islamic Republic of Iran (172 030 new cases; 17% decrease), and Turkey (158 236 new cases; 6% increase).

Globally, cases of the Alpha variant have been reported in 193 countries, territories or areas (hereafter countries; no new country added since last week), while 142 countries (one new country since last week) have reported cases of the Beta variant; and 96 countries (four new countries since last week) have reported cases of the Gamma variant. For the Delta variant, since it was first reported in October 2020, it has been reported in 180 (six new countries since last week) countries across all six WHO regions as of 14 September.

Special Focus: Update on SARS-CoV-2 Variants of Interest and Variants of Concern
WHO, in collaboration with national authorities, institutions and researchers, routinely assesses if variants of SARS-CoV-2 alter transmission or disease characteristics, or impact vaccine, therapeutics, diagnostics or effectiveness of public health and social measures (PHSM) applied by national authorities to control disease spread.” Signals” of potential Varients of Concern(VOCs) of Variants of Intrest (VOIs) are detected and assessed based on the risk posed to global public health.
As variants evolve, WHO will continue to update lists of global VOIs and VOCs to support setting priorities for surveillance and research, and ultimately guide response strategies (for more information, please see th
 e Tracking SARS-CoV-2 variants website).
e Tracking SARS-CoV-2 variants website).
National authorities may choose to designate other variants of local interest/concern and are encouraged to investigate and report on the impacts of these variants.
As surveillance activities to detect SARS-CoV-2 variants are strengthened at national and subnational levels, including through the expansion of genomic sequencing capacities, the number of countries, territories or areas (hereafter countries) reporting VOCs continues to increase (Figure 4, Annex 1). This distribution should nonetheless be interpreted with due consideration of surveillance limitations, including differences in sequencing capacities and sampling strategies between countries.
As countries gradually resume non-essential international travel, the introduction of risk mitigation measures aiming to reduce travel-associated exportation, importation and onward transmission of SARS-CoV-2 should be based on thorough risk assessments conducted systematically and routinely.
Special Focus: COVID-19 in children and adolescents
SARS-CoV-2 infections among children and adolescents typically cause less severe illness and fewer deaths as compared to adults. While a less severe course of disease is a positive outcome, there are concerns that mild symptoms may have led to less testing, resulting in fewer identified cases of SARS-CoV-2 infection in children and adolescents. If children and adolescents with mild or no symptoms also transmit the disease, they may also contribute to transmission in the community. Consequently, understanding symptoms, infectivity and patterns of SARS-CoV-2 transmission in children and adolescents is essential for developing, adapting and improving control measures for COVID-19 across all ages, especially since vaccination is not currently available or authorized for those under the age of 12 years in most contexts.
This report summarizes the current knowledge around SARS-CoV-2 infection acquisition and transmission and COVID-19 disease in children under the age of five years, older children (5 to 9 years old), younger adolescents (10 to 14 years old) and older adolescents (15 to 19 years old). Some information on incidence and mortality is also provided for young adults (20 to 24 years old). It aims to inform decisions, based on local contexts, on how best to keep schools, kindergarten and day-care facilities open and what advice to apply to intergenerational mixing.
Incidence and mortality in children, adolescents and young adults
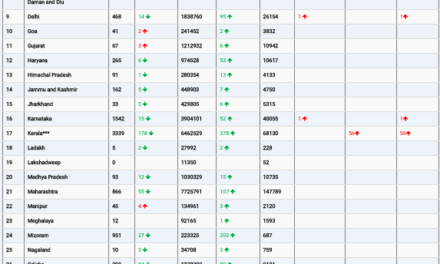
Overall, there are proportionally fewer cases and deaths from COVID-19 among children, adolescents and young adults as compared to adults (Table 1). Based on age-disaggregated case data reported to WHO from 30 December 2019 to 6 September 20211, the proportion of global cases increased with age category: children under the age of five represented the smallest proportion of cases among individuals up to 24 years old, while older adolescents (15 to 19 years old) and young adults (20 to 24 years old) grouped together had the highest proportion of the global cases. Deaths for all age groups represented less than 0.5% of the proportion of global deaths.

What are the symptoms of COVID-19 in children and adolescents?
Younger children (under five years old), older children and adolescents (10 to 19 years old) usually have fewer and milder symptoms of SARS-CoV-2 infection than adults >25 years old and are less likely than adults to experience severe COVID-19. Milder symptoms and asymptomatic presentation often mean less frequent care-seeking for these groups; thus, children and adolescents tend to be tested less frequently and cases may go unreported. Early reports suggested an age-dependent risk of severe disease with those under one year experiencing more severe disease, although several reviews show that neonates (first 28 days of life) have the mild disease as compared to other paediatric patients. However, it is important to note that children under the age of one year and within the neonatal period (first 28 days after birth) have a higher risk of diseases which have an overlapping presentation with COVID-19, such as pneumonia and malaria. Additionally, age disaggregation has not been systematically provided in the current literature and the results of these studies are context-specific such as timing within the pandemic and an emphasis on hospitalized patients.
Children and adolescents can experience prolonged clinical symptoms (known as post COVID-19 condition, or post-acute sequelae of SARS-CoV-2 infection), however, the frequency and characteristics of these are still under investigation.
Additionally, a hyperinflammatory syndrome, referred to as paediatric inflammatory multisystem syndrome,
temporally associated with SARS-CoV-2 (PIMS-TS) in Europe and multisystem inflammatory syndrome in
children (MIS-C) in the United States of America, although rare, can occur, and complicates recovery from COVID-19 . The severity of disease in children and adolescents caused by SARS-CoV-2 variants of concern (VOC), in comparison with non-VOC lineages, remains under investigation.
Are children and adolescents less susceptible to SARS-CoV-2 infection than adults?
The risk of becoming infected with SARS-CoV-2 depends on a combination of susceptibility (host biological factors), biological properties of the virus, environmental factors associated with exposure type (going to work, or school etc.) and exposure intensity (level of community transmission and adherence to public health and social measures (PHSM)).
Multiple population-based SARS-CoV-2 seroprevalences and viral shedding studies have investigated whether children and adolescents are infected at the same rate as adults, but the results have been mixed, possibly because of the studies being conducted at different time points in the pandemic when populations were subjected to different levels of PHSM. Even so, we do know that children of all ages can become infected and can spread the virus to others.
Data on the global incidence of COVID-19 in adolescents suggests they test positive for SARS-CoV-2 at a higher proportion than children, however, seroprevalence surveys are needed to provide more information. Additionally, more detailed epidemiological information about the factors influencing the susceptibility of children and adolescents to the new SARS-CoV-2 variants is urgently needed.
What about the transmission of infection? Is there a difference between young children, older children and adolescents in transmitting SARS-CoV-2?
Outbreaks of COVID-19 have been identified in secondary schools, summer camps and day care centres, particularly when neither physical distancing nor masks were used to reduce risk. There is some preliminary evidence that children may be less infectious, than adolescents and adults, as measured by secondary attack rates.
Children and adolescents who become infected with SARS-CoV-2 shed the virus in their respiratory tract and may also shed virus in their faeces. Among individuals who were positive for SARS-CoV-2 who were tested at the same time point after symptom onset, SARS-CoV-2 viral RNA shedding in the respiratory track appeared similar in children, adolescents and adults.
The relationship between age, viral load and transmission across the full symptom spectrum of SARS-CoV-2 infection has not been comprehensively investigated because people with no, or mild, symptoms are seldom tested systematically.
Thus, the relative transmissibility of SARS-CoV-2 at different ages remains uncertain, largely due to the challenges involved in disentangling the influences of biological, host, virus and environmental factors.
Conclusions
Children and adolescents infected with SARS-CoV-2 generally present with milder symptoms of COVID-19 disease; although infection with the variants of SARS CoV-2, including the Delta variant, require more investigation to determine if this will remain the case. The risk of transmission to and from children and adolescents depends on contextual factors such as the level of community transmission and the measures implemented to control the virus, host factors in the child, as well as biological factors related to the virus itself. However, children and adolescents of all ages become infected and also transmit SARS-CoV-2 to others. Younger children may be less susceptible than older children and adolescents, but the precise role of children and adolescents in the overall transmission of SARS-CoV-2 still requires further investigation.
The use of public health and social measures (PHSM), including physical distancing, cleaning hands, coughing into a bent elbow or a tissue, adequate ventilation in indoor settings, and masks (for older children – see guidance below), should be consistently and appropriately implemented for all ages in schools, especially since children under the age of 12 years are generally not yet eligible for vaccination.
Resources: WHO guidance and reports on COVID-19 and children and adolescents
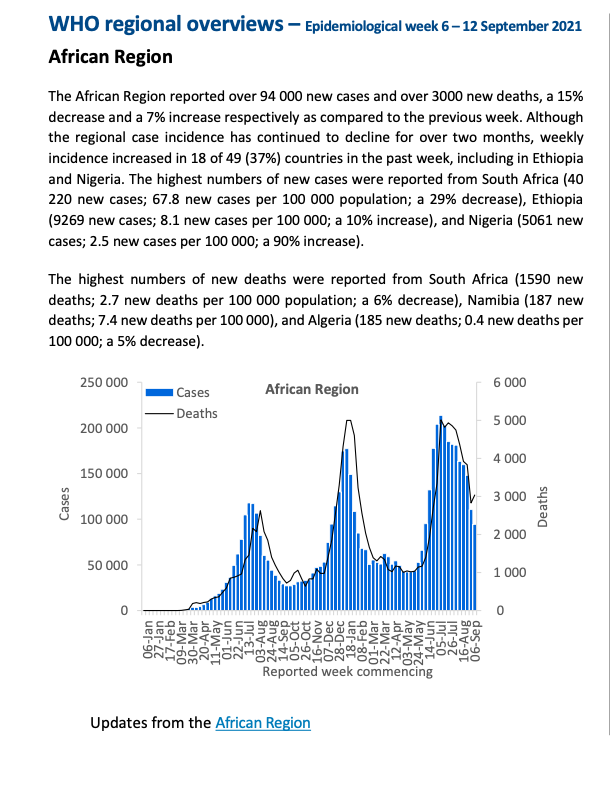
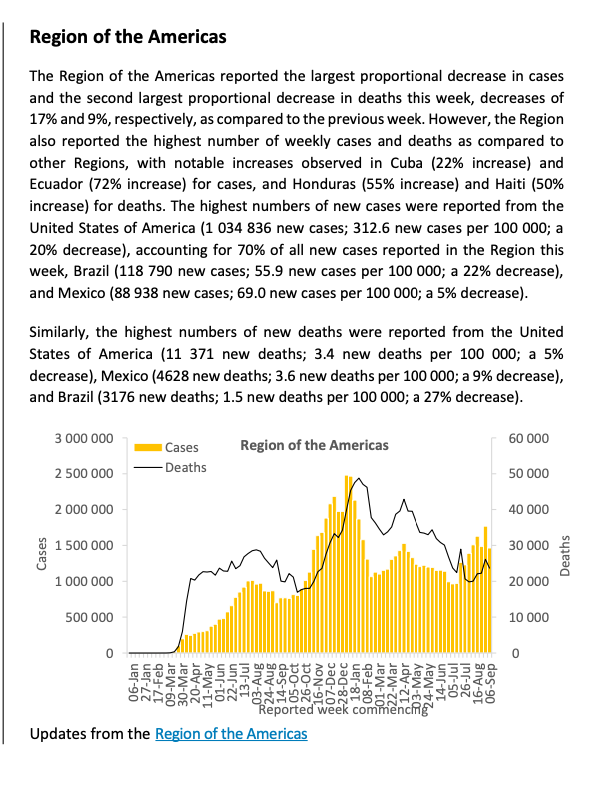
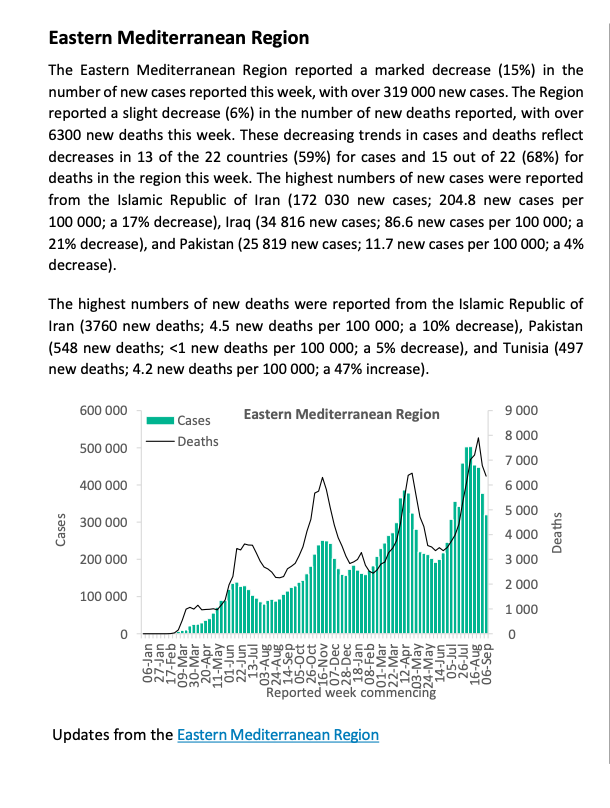
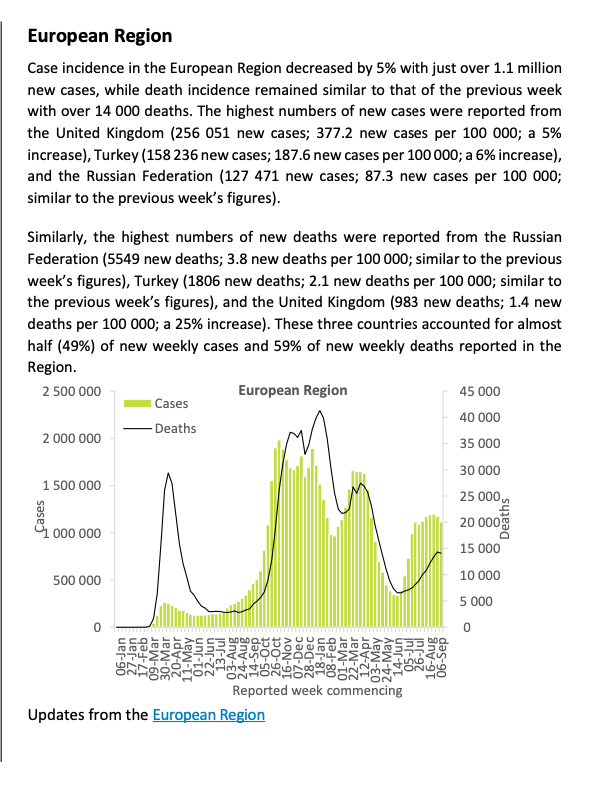
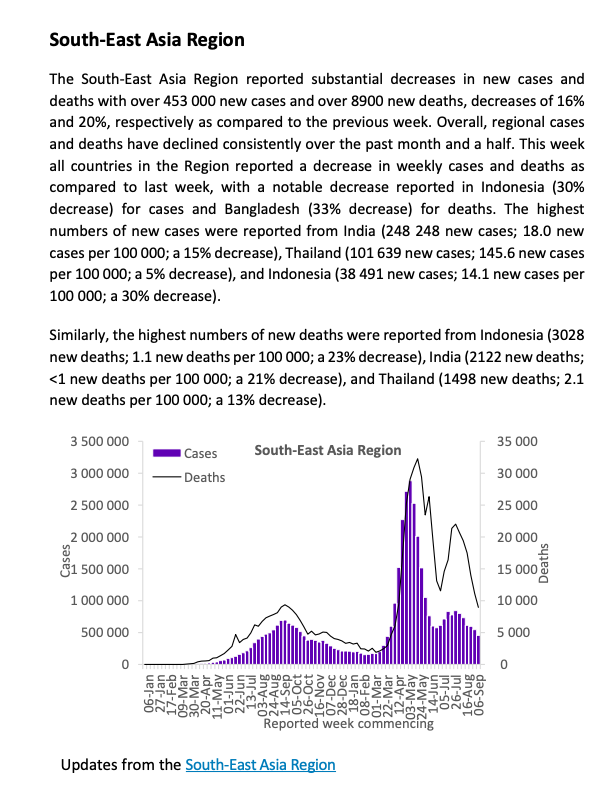
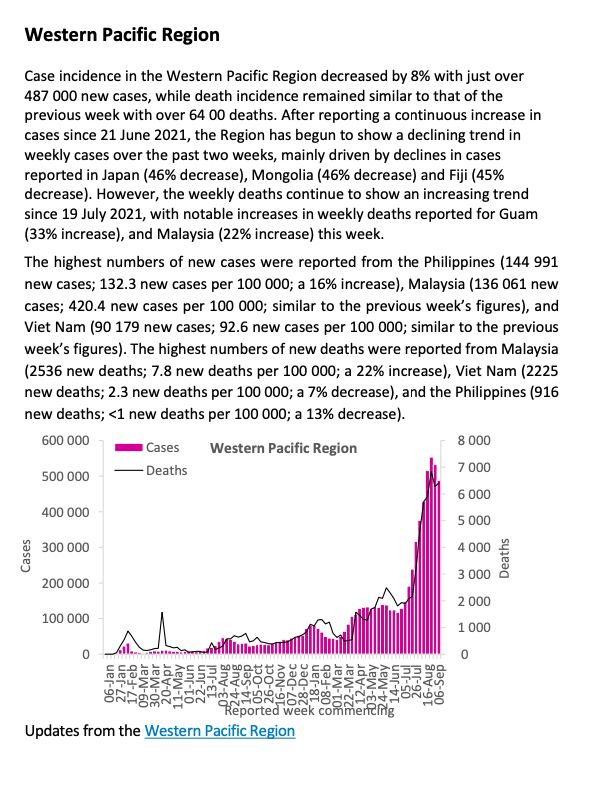
WHO regional overviews – Epidemiological week 6 – 12 September 2021