Boston, MA – March 5, 2025 – A groundbreaking study suggests that modifying macrophages in the lungs could potentially prevent pulmonary hypertension, a condition marked by high blood pressure in lung arteries that can lead to heart failure.
Pulmonary hypertension has long been a challenge in neonatology. In the 1980s, mortality rates for newborns with the disease were as high as 85%, but advances in treatment—such as inhaled nitric oxide, mechanical ventilation improvements, and extracorporeal membrane oxygenation (ECMO)—have drastically improved survival rates. However, the condition still persists without a cure.
Dr. Stella Kourembanas, chief of the Division of Newborn Medicine at Boston Children’s Hospital, has spent decades researching pulmonary hypertension and its links to inflammation. Her team’s latest findings, recently published in Arteriosclerosis, Thrombosis, and Vascular Biology, indicate that early intervention targeting macrophages could be key to preventing disease progression.
The Role of Macrophages in Pulmonary Hypertension
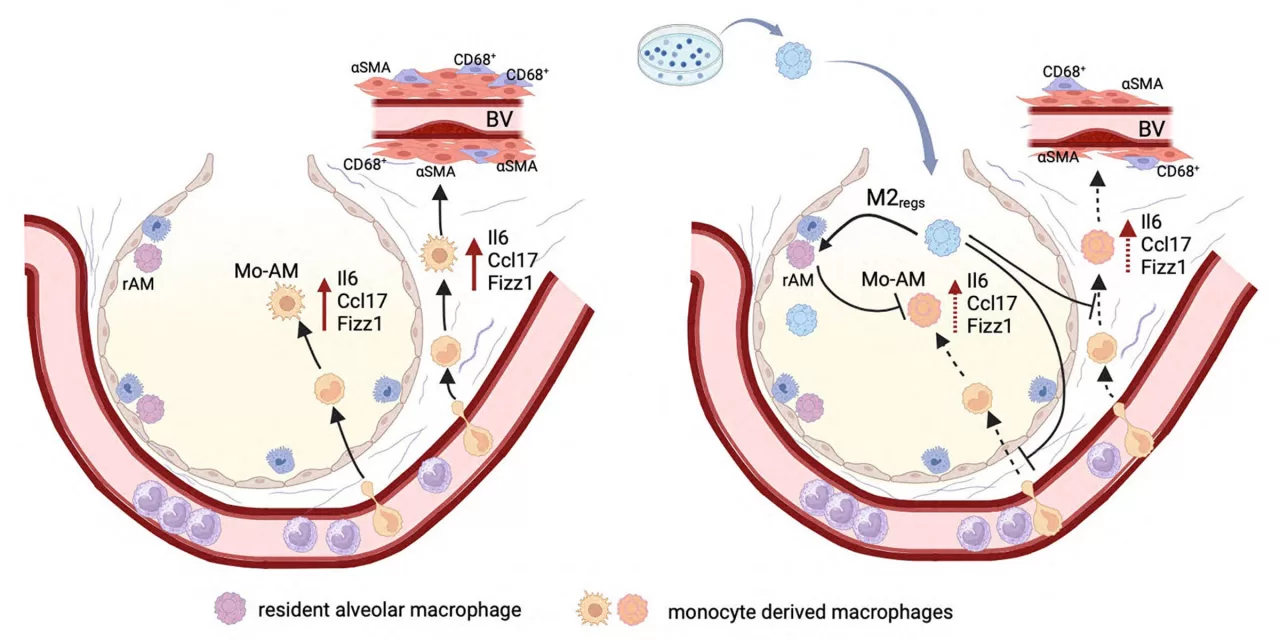
Macrophages, a type of white blood cell, play a dual role in pulmonary hypertension. Some macrophages promote inflammation, leading to vascular disease, while others have anti-inflammatory properties that help resolve inflammation. Kourembanas’ research has focused on shifting the balance towards the latter.
By incubating macrophages with specific cytokines to give them an anti-inflammatory profile, Kourembanas’ team was able to significantly reduce inflammation in mice exposed to hypoxia—a key factor in pulmonary hypertension. When these modified macrophages were delivered into the lungs, inflammation decreased, monocyte recruitment was halted, and four weeks later, heart and vascular complications were reduced.
“The key is to halt inflammation at an early stage before it triggers a cascade of vascular remodeling that ultimately forces the heart to work harder,” explains Angeles Fernandez-Gonzalez, Ph.D., the study’s lead author.
Future Therapeutic Possibilities
If this macrophage-focused therapy translates to human treatment, it could provide a major breakthrough for infants with bronchopulmonary dysplasia (BPD), a condition that arrests lung development and increases the risk of pulmonary hypertension. Currently, steroids are used to reduce inflammation, but they also hinder normal lung development. A macrophage-based therapy could offer an alternative with fewer side effects.
Potential therapeutic approaches include cell therapy using modified macrophages, delivering macrophage-derived factors, or altering the lung environment to sustain anti-inflammatory macrophages. However, researchers acknowledge challenges in ensuring that beneficial macrophages maintain their properties once introduced into the lung.
“It may turn out not to be cells themselves but something derived from them that has long-lasting effects,” Kourembanas says. “Ongoing research and future clinical trials will provide the answers.”
Looking Ahead
The research highlights the importance of inflammation in the early stages of pulmonary hypertension and opens new avenues for targeted therapies. While more studies are needed to determine safety and efficacy in humans, the findings mark a promising step toward preventing and managing this complex disease.
Disclaimer: This article summarizes ongoing research and should not be considered medical advice. Clinical applications of macrophage-based therapy are still under investigation, and further studies are required to confirm safety and efficacy in human subjects.