Millions of people with type 2 diabetes could soon receive more effective treatment, thanks to a groundbreaking, low-cost tool developed by researchers at the University of Exeter. Announced at the Diabetes UK Professional Conference 2025 and published in The Lancet, this innovative tool predicts which glucose-lowering drug will work best for individual patients, potentially transforming diabetes care worldwide.
A Personalized Approach to Diabetes Management
Managing blood glucose levels is crucial in preventing severe diabetes-related complications. However, only about a third of people with type 2 diabetes achieve optimal blood sugar control. This struggle contributes to devastating health effects and places a significant financial burden on the UK’s healthcare system, costing an estimated £6.2 billion annually.
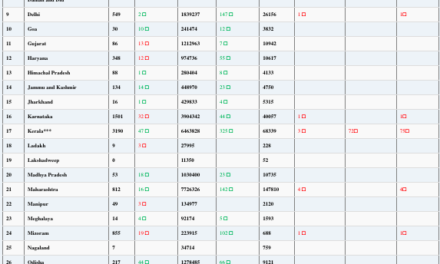
The newly developed tool aims to address this challenge by offering a personalized approach to treatment. Using data from one million patients in the UK, it predicts which glucose-lowering drug will provide the best results for an individual, reducing the need for a trial-and-error approach.
The Impact of the New Tool
The tool was designed to help doctors determine the most effective treatment option beyond metformin, which is the standard first-line medication. Currently, there are five major classes of glucose-lowering drugs, but their effectiveness varies significantly between individuals. Until now, choosing the right medication has been largely uncertain.
Key findings from the research include:
- Only 18% of people with type 2 diabetes in the UK are currently on the most effective glucose-lowering drug for their condition.
- Patients using the tool’s recommendations could see an average reduction of 5 mmol/mol in HbA1c levels after one year.
- This improvement could significantly delay the need for additional diabetes medications.
- The tool is expected to lower the risks of severe complications, including heart attacks, strokes, and kidney disease.
A Cost-Effective and Immediate Solution
Unlike costly new drug developments, this tool relies on routinely collected clinical data, making it an easily implementable and cost-free addition to diabetes care. By incorporating common health metrics such as sex, weight, and standard blood tests, it provides an accessible and effective method to tailor treatment plans.
Professor John Dennis, lead researcher from the University of Exeter, emphasized the potential impact of this innovation: “For the first time, our model allows people living with type 2 diabetes to quickly identify the best treatment to manage their blood sugar levels, helping reduce their risk of diabetes complications. This offers a major advance on the current approach to choosing diabetes medications.”
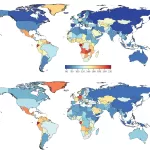
Future Implementation and Global Reach
Currently, the tool’s effectiveness is being tested in real-world settings with 22,500 patients across Scotland. These trials will determine how best to integrate the tool into clinical practice in the UK and beyond.
Professor Andrew Hattersley, a senior researcher at the University of Exeter, highlighted its immediate applicability: “Our model can be implemented in clinical care immediately and at no additional cost. We hope to roll it out quickly to help people with type 2 diabetes in the UK and globally.”
Dr. Elizabeth Robertson, Director of Research and Clinical at Diabetes UK, also praised the tool’s potential: “If shown to be effective in practice and widely adopted, this innovation could mark the most significant advance in type 2 diabetes care in over a decade.”
A Step Towards Precision Medicine
Dr. Adam Babbs, Head of Translation at the Medical Research Council, which co-funded the study, stated: “This is a trailblazing example of precision medicine, ensuring that the right patient receives the right therapy at the right time. The potential benefits for both patients and healthcare systems are immense.”
With promising results and growing interest from the medical community, this tool could soon redefine diabetes management worldwide, offering hope for millions struggling with the condition.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. Patients should consult their healthcare providers before making any changes to their treatment plans.