The global AIDS response is not only off-the-target but also slipping by leaps and bounds in some countries or for some communities.
All governments promised to end AIDS by 2030 by committing to the UN Sustainable Development Goals (SDGs) a decade back “where no one is left behind.” Undeniably, a lot of progress took place in preventing new HIV infections and helping millions of those living with the virus lead a healthy life worldwide. But this progress is no excuse for complacency or must not be allowed to paralyse us in urgently addressing the acute need of scaling up people-centred and rights-based responses.
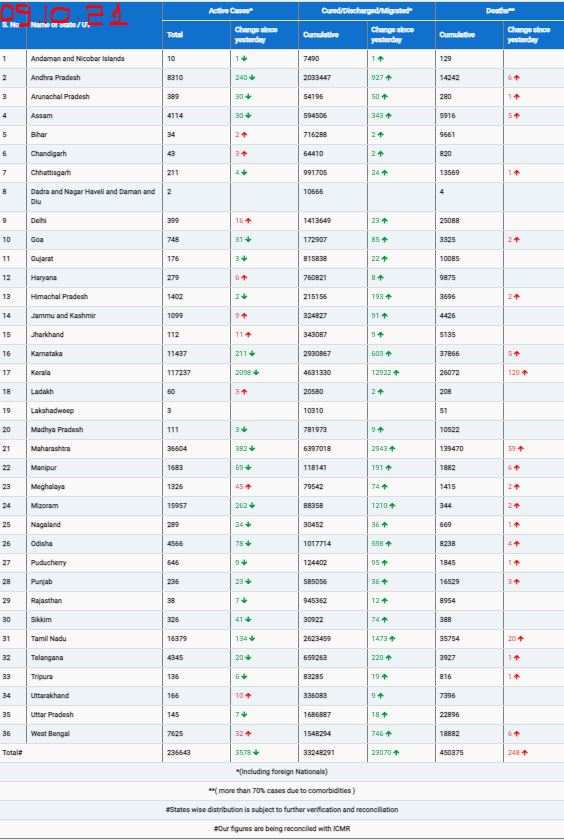
Despite having a range of evidence-based HIV prevention tools, the world saw 1.3 million new people getting diagnosed with HIV in 2023. This is over three times more new infections than what was promised: Leaders had pledged to reduce annual new infections to below 370,000 by 2025.
Despite having best of HIV treatment options to keep people with HIV healthy and well, over 630,000 people died of AIDS-related illnesses in 2023. Compared to 2010 when 1.3 million people died of AIDS-related illnesses, the rate has halved by 2023 -but the number of lost lives in 2023 is 2.5 times more than what our leaders promised to achieve by 2025 (that deaths due to AIDS-related illnesses by 2025 should be less than 250,000).
Acute urgency for accelerating rights-based AIDS response
“Every new HIV infection or a death due to AIDS-related illness is a grim reminder that we could have done better to prevent HIV or on treatment, care and support. It is high time for accountability, review and course correction so that we all can get on track to end AIDS and keep all the promises enshrined in the SDGs,” said Dr Ishwar Gilada who is the longest serving HIV medical expert in India, is twice elected to the Governing Council of International AIDS Society (IAS) and Chairs IAS Asia Pacific.
“I think globally, regionally and here in India, we do have a choice. We can act now to end AIDS as a public health threat by 2030. We can actively work to keep people living with HIV on treatment and healthy. We can accelerate efforts to reduce new infections substantially and we can almost eradicate AIDS-related deaths. But to do so, we all will require firmer commitment by leaders to invest in effective programmes that engages community, further reduces stigma and discrimination, and addresses sustainability in the integration of the response. There is a pathway to ending AIDS, and we have a map. But are we bold enough to follow it and accelerate our progress?” said David Bridger, UNAIDS India Director at the 16th National Conference of AIDS Society of India (ASICON 2025).
The deadly gap: Promise vs reality
If every life counts, then we have to deliver on AIDS targets as well as all other SDGs. No excuse for inaction.
Some of the AIDS-related promises of our world leaders for 2025 are to ensure that:
* 95% of people at risk of HIV are using combination prevention options
* 95% of people with HIV know their HIV positive status
* 95% of those who know their HIV positive status are receiving lifesaving antiretroviral treatment
* 95% of those on treatment remain virally suppressed
* 95% of women access sexual and reproductive health services
* 95% of HIV positive pregnant women are receiving full services to prevent vertical transmission of HIV (during pregnancy, child birth and breastfeeding)
* 90% of people living with HIV are receiving TB preventive therapy
* 90% of people living with HIV and people at riskare linked to other integrated health services
* Less than 10% of people living with HIV and key populations experience stigma and discrimination
* Less than 10% of people living with HIV, women and girls and key populations experience gender-based inequalities and violence
* Less than 10% of countries have punitive laws and policies
Why are we failing to do what we know works!
The latest Global AIDS Update Report of the UNAIDS shows that most new HIV transmissions are attributed to among those who are undiagnosed, followed by those who are diagnosed but untreated, and then by those who are on antiretroviral therapy but not virally suppressed. There is “zero risk” of HIV transmission from those who are on treatment and virally suppressed or those whose viral load is undetectable (that is why it is referred to as undetectable equals untransmittable or U equals U).
To deliver on the 2025 targets, instead of 95% of people living with HIV knowing their status, only 78% were aware of it by 2023 in Asia Pacific. Instead of 90% of those knowing their status receiving the lifesaving antiretroviral therapy by 2023, only 67% were getting the medicines in the region. And instead of 86% of those on antiretroviral therapy remaining virally suppressed, only 65% were virally suppressed in the region by 2023.
“The alarming point is that in the Asia Pacific region, nearly a third of people living with HIV are not getting the care and support they need to stay healthy and prevent transmission” said UNAIDS India leader David Bridger. “Asia Pacific has the second largest epidemic globally.”
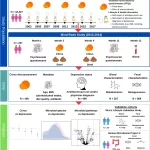
Six countries in the Asia Pacific region have growing HIV epidemics: Bangladesh, Lau, Papua New Guinea, Afghanistan, Fiji, and the Philippines. In the Philippines HIV rates have increased by almost 600% during 2010-2023 (largely driven by male to male sex, predominantly among younger people). In the Fiji, HIV rates grew by over 200% during 2010-2023, largely driven by injecting drug use.
Nine countries of the region have increasing number of deaths due to AIDS-related illnesses: Pakistan, Indonesia, and Mongolia along with the above six countries where HIV rates are on a rise too.
However, some countries are doing better too to meet 2025 targets. These countries include: Cambodia, Nepal, New Zealand, and Thailand where over 80% of people living with HIV know their status, receive antiretroviral treatment and are virally suppressed.
Only 1 country in Asia Pacific has been able to keep the HIV prevention promise: Nepal.
Four countries in Asia Pacific region have eliminated vertical transmission of HIV: Malaysia, Maldives, Sri Lanka and Thailand.
Why are we not-doing-all-what-we-can on HIV prevention?
“Prevention efforts are not as powerfully being upheld. Only Nepal is on course to reach the target of 90% decline in new HIV infections by 2030,” said David. “In India, annual new HIV infections have declined by 44% during 2010-2023. We need far more acceleration of HIV prevention efforts here in India.”
“In 2024-2025, 84% of estimated people living with HIV in India were aware of their status, 86% of them were on lifesaving antiretroviral therapy, and 94% of them were virally suppressed,” said Dr Uday Bhanu Das of Indian government’s national AIDS programme (formally called as National AIDS Control Organisation (NACO), Ministry of Health and Family Welfare, Government of India).
Globally, 86% people living with HIV knew their status, 89% were on antiretroviral therapy, and 93% of those on antiretroviral therapy were virally suppressed in 2023.
Why ending AIDS in Asia Pacific and India is critical
“For the world to end AIDS, we must get it right here in Asia and the Pacific, but also in India because India has the second largest number of people living with HIV outside of South Africa,” said David.
Asia Pacific accounts for a quarter of the new HIV infections in the world: 300,000 new HIV infections in the region out of the total 1.3 million new infections worldwide in 2023. India accounted for 5-6% of the total new HIV infections globally in 2023.
If data alone does not drive the point home, then read this:
* Every 2 minutes in Asia Pacific region, one person is newly infected with HIV.
* Every hour this represents 35 people newly infected, including 9 young people.
* Every day, 300 men who have sex with men, 80 people who inject drugs, 50 sex workers and 15 transgender people become newly infected.
* Every hour 17 people die of an AIDS-related illness.
* And every day we lose 9 young people between the ages of 15 to 24 to AIDS-related illnesses in the region.
Key populations are key to HIV response
“HIV is concentrated among key populations and their partners. In 2022 in the Asia Pacific region, 4 out of every 5 new infections were among key populations and their sexual partners. This translates to nearly 80% of new infections were among key populations and their sexual partners. Of this, 43% were through male to male sex, which is an increase of over 34% over the past 10 years,” said David.
“Access to combination HIV prevention services among key populations throughout the region remains limited. HIV service coverage is near 47% for female sex workers, 31% for men who have sex with men, 34% for transgendered people and only 21% for people who inject drugs,” he added. “However, 9 countries in the region spend less than 15% of HIV budget on key population focussed programming.”
Pre-Exposure Prophylaxis (PrEP – a medicine taken to reduce the risk of HIV acquisition) has been available since 2012 (when US FDA had first approved it), but uptake is low in the region (2.5% of 2025 target): In 2023, only 204,000 people had used PrEP in Asia Pacific whereas the target was to reach over 8.2 million people by 2025.
Take the rights path
David calls on governments for “renewing and intensifying focus on key populations” in terms of HIV response, health and social security. “We need to refocus and ensure that we are targeting the right populations with the right interventions in the right places – and – we are doing this at scale that will have the impact.”
“We need to modernise service delivery. This means adopting innovations, and using HIV combination prevention tools to their fullest – this includes PrEP, long-term injectables and HIV self testing. We also need to eliminate barriers to equitable HIV programme coverage which includes addressing legal and structural barriers that are fuelling stigma and discrimination,” he said. “We must invest more in HIV prevention and community-led programming.”
Bobby Ramakant – CNS