A recent study published in JAMA Surgery on February 19, 2025, highlights the long-term advantages of Roux-en-Y gastric bypass (RYGB) over sleeve gastrectomy (SG) in terms of excess body mass index loss (percentEBMIL) after 10 years. The study, conducted by Dr. Marko Kraljević and colleagues at the University Hospital of Basel, Switzerland, provides critical insights into the effectiveness of these two popular bariatric procedures.
Study Overview
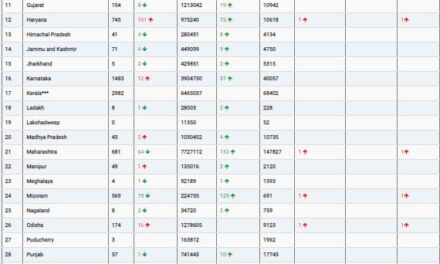
The Swiss Multicenter Bypass or Sleeve Study, a randomized clinical trial, included 217 patients who were assigned to undergo either SG (107 patients) or RYGB (110 patients). Researchers examined various outcomes, including weight loss, metabolic improvements, reoperation rates, and quality of life assessments, over a decade.
Key Findings
In the intention-to-treat (ITT) analysis, the mean percentEBMIL between the two procedures was comparable (60.6% for SG vs. 65.2% for RYGB), indicating no statistically significant difference. However, patients who underwent SG had a markedly higher conversion rate (29.9%) due to inadequate weight loss or gastroesophageal reflux compared to RYGB patients (5.5%).
When analyzing per protocol (PP) data, which excludes patients who required additional surgical intervention or deviated from the assigned procedure, RYGB demonstrated a significantly higher mean percentEBMIL (65.9%) compared to SG (56.1%). Nevertheless, total weight loss percentages were relatively close (27.7% for RYGB vs. 25.5% for SG). Additionally, SG patients experienced significantly higher rates of new-onset gastroesophageal reflux than those who underwent RYGB.
Clinical Implications
The study underscores the long-term benefits of RYGB for sustained weight loss, particularly in patients who strictly adhered to their assigned procedure. However, both procedures were effective in achieving significant weight reduction and metabolic improvement. The findings highlight the importance of personalized treatment planning based on individual patient needs, considering factors such as reflux risk and the likelihood of additional surgeries.
Disclosures
Several authors of the study disclosed affiliations with the pharmaceutical and medical device industries, emphasizing the need for independent validation of these findings.
More information on this study can be found in JAMA Surgery: DOI: 10.1001/jamasurg.2024.7052.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. Patients considering bariatric surgery should consult with a qualified healthcare provider to discuss the best treatment options for their specific conditions.