WHO has documented over 2254 attacks on health care in Ukraine since the start of full-scale war in the country 3 years ago. The health-care system continues to face unprecedented challenges. In 2025, attacks on health care have not stopped and we continue to document them almost daily. Forty-two attacks have already been recorded in 2025, resulting in 12 injuries and 3 deaths. An overnight strike in Odesa, which damaged the region’s largest and most innovative children’s clinic, disrupting vital services, fits this ongoing and alarming pattern. This attack highlights the constant risks and obstacles facing health-care workers, as well as the persistent interruptions in the delivery of medical services across Ukraine.
“Being a doctor in wartime means returning home after each shift, wishing the war had never happened and praying for its swift end. People are exhausted – both the patients and the health-care workers. Yet, as medical professionals, we do not have the luxury of being tired. Our patients need us to keep going and we must push through the fatigue to continue delivering the care they deserve,” says Olha Zavyalova, emergency physician and surgeon from the Dnipro region.
Shifting health needs
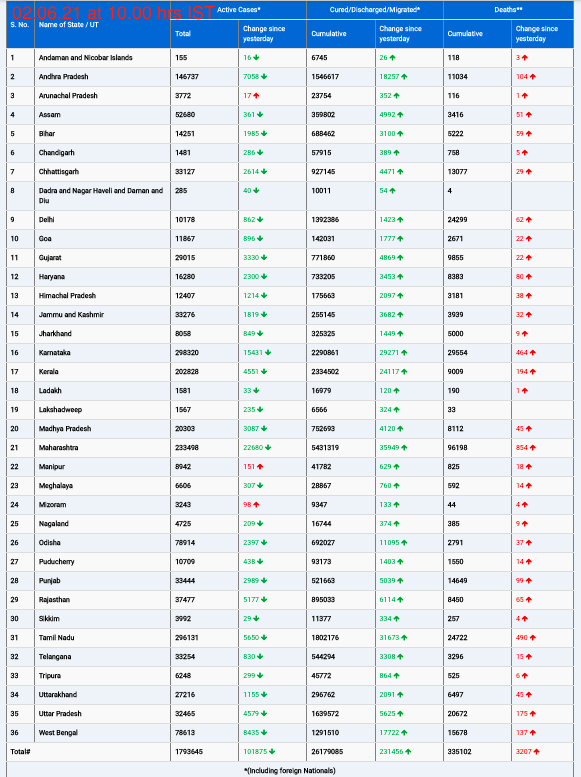
Three years of full-scale war and 11 years of invasion have had a profound impact on health across Ukraine. According to the latest WHO Ukraine health needs assessment (October 2024), 68% of Ukrainians report a decline in their health compared to the pre-war period. The most prevalent health issues are mental health concerns, with 46% of people affected, followed by mental health disorders (41%) and neurological disorders (39%).
Noncommunicable diseases (NCDs) account for 84% of all deaths in Ukraine. The primary barriers to care for NCD patients are unavailability of services and high cost of medicines, leaving those with chronic conditions vulnerable to disruption in care and irreversible health deterioration.
The war has intensified health needs, particularly in areas such as trauma care and rehabilitation. The Ministry of Health estimates that by mid-2024, 100 000 amputations had been performed due to the war. The severe shortage of trauma specialists, prosthetics and rehabilitation services has further exacerbated the crisis. Healing is often a matter of time but can also be a matter of opportunity. Long-term rehabilitation services for war-injured people will be essential for both physical and psychological recovery.
Building a resilient health system
WHO is addressing Ukraine’s growing health needs, working to ensure access to quality health care for all Ukrainians, with a focus on strengthening primary health care to combat the prevalence of NCDs and expanding access to vital mental health and rehabilitation services. We are also supporting building a resilient health system by collaborating with the Ministry of Health and the National Health Service of Ukraine to update reimbursement packages, including rehabilitation, and standardize assessment tools. This ensures that resources are allocated where needed most, laying a stronger foundation for quality care.
Key achievements on mental health include developing the Target Model of the Mental Health and Psychosocial Support System of Ukraine and the 2024–2026 National Mental Health Action Plan, along with 24 oblast-level plans. Rehabilitation is a key highlight for our efforts in building the capacity of professionals. By the end of 2024, WHO conducted training for multidisciplinary rehabilitation teams from 28 non-specialized inpatient rehabilitation departments from 11 oblasts.
A key milestone was the reform of Ukraine’s stroke care system, with WHO leading technical discussions, conducting clinical audits and supporting the monitoring of over 50 health-care facilities to improve acute care. WHO also introduced the Package of essential NCD interventions, emphasizing integrated care for low-resource settings. On antimicrobial resistance, the National Action Plan was approved, with ongoing training for health-care workers and facility modernization. WHO also supported primary health-care financing through costing exercises, payment design and network development, culminating in the Ministry of Health’s approval of a capitation rate methodology in July 2024.
Displacement and vulnerability
Access to health care remains a critical issue across Ukraine. One in 4 people (25%) report a decrease in access to medical services since the start of the full-scale invasion in February 2022. The cost of medicines and treatment continues to be a major barrier to care, with 35% of people in October 2024 indicating that they had postponed medical care due to financial challenges.
Internally displaced persons (IDPs) are among the most vulnerable groups. Thirteen percent of IDPs lack access to primary health-care facilities, compared to just 6% among host communities. Similarly, 9% of IDPs have no access to a family doctor (compared to 4% of locals) and 12% have not signed a declaration with a family doctor, compared to 5% in host communities. While IDPs report better changes in health-care quality than locals, their access to primary care and preventive services remains lower.
Health-care access is increasingly unequal, particularly in front-line areas. The most damaged and dysfunctional health-care facilities are located along the front line, where the remaining population often faces multiple vulnerabilities, including being elderly or living with disabilities. These facilities suffer from frequent disruptions in medical supplies, shortages of health-care workers and significant barriers to care. In 10 front-line oblasts, 68% of adults report worsening health. Health-care refusal rates are highest in Kherson (43%), followed by Kharkiv (24%) and Zaporizhzhia (18%). The continued disruptions in these areas underscore the urgent need for sustained support and interventions.
WHO efforts: response, recovery and reforms
Last year, WHO shifted focus from emergency relief to capacity building, prioritizing primary care and critical areas such as NCDs, immunizations, mental health, HIV, tuberculosis, infection control and addressing antimicrobial resistance. WHO is collaborating with Ukrainian authorities to enhance health responses and recovery efforts, including the installation of 29 modular primary health clinics in affected regions. WHO is also supporting health finance reforms, including capacity building, procurement transparency and strategic planning to strengthen Ukraine’s health system, ensuring that it remains resilient amid ongoing challenges. In addition, professional development opportunities for nurses and health-care workers are being expanded to address workforce shortages and bolster the overall health system.
Looking ahead: rebuilding health, restoring hope
Health is the foundation of peace and recovery. Rebuilding health systems means restoring hope, dignity and securing the future. At WHO, we are acting now – we do not wait for the war to end. We are engaged in recovery, response and reforms simultaneously. Every delayed intervention worsens the situation and increases future costs. That is why we call on our international partners: more than ever, we need your support now. Together, we can ensure that no one in Ukraine is left behind.