Researchers at ETH Zurich have made a groundbreaking discovery in the field of targeted drug delivery, uncovering the precise mechanism by which microbubbles, activated by ultrasound, facilitate drug penetration into cells. For the first time, they have visualized how liquid microjets, created by vibrating microbubbles, puncture the cell membrane, allowing drug uptake.
Overcoming the Blood-Brain Barrier
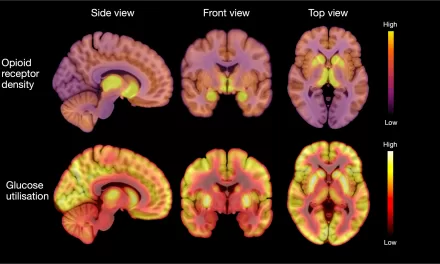
The treatment of neurological diseases such as Alzheimer’s, Parkinson’s, and brain tumors presents a significant challenge due to the brain’s natural protective mechanism, the blood-brain barrier. This barrier restricts the entry of foreign substances, including many therapeutic drugs. To address this, researchers are exploring innovative methods to deliver drugs through the bloodstream while ensuring precision and safety.
One promising approach involves the use of microbubbles—gas-filled spheres smaller than red blood cells, stabilized by a lipid coating. When injected into the bloodstream alongside medication, these microbubbles can be activated by ultrasound, creating tiny openings in the cell membrane of blood vessel walls, allowing the drug to pass through.
Breakthrough in Visualization
Until now, the exact process by which microbubbles create these pores remained unclear. A research team led by Professor Outi Supponen at ETH Zurich’s Institute of Fluid Dynamics has now successfully demonstrated this mechanism. “We were able to show that under ultrasound, the surface of the microbubbles loses its shape, leading to the formation of microjets—high-speed liquid streams that puncture the cell membrane,” explained Marco Cattaneo, a doctoral student and lead author of the study published in Nature Physics.
Microjets at 200 kph: A Powerful Yet Gentle Mechanism
Observing this process was a major challenge due to the rapid oscillation of microbubbles—up to several million times per second. Traditional top-view microscopy methods were insufficient, as they did not capture the crucial interaction between the microbubble and the cell. To overcome this, the researchers designed a specialized microscope with 200x magnification and coupled it with a high-speed camera capable of capturing ten million images per second.
Their experiments, conducted using an in-vitro blood vessel model, revealed that at a specific ultrasound pressure, microbubbles stop oscillating in a spherical pattern and instead form lobed shapes. As these lobes collapse inward, they generate powerful microjets traveling at speeds of up to 200 kph. These jets pierce the cell membrane without causing widespread damage, enabling the drug to enter the targeted cells effectively. Remarkably, this jetting process does not destroy the bubble, meaning it can repeat with each ultrasound cycle, enhancing drug delivery efficiency.
Implications for Future Treatments
One of the study’s key findings is that these microjets can be generated at relatively low ultrasound pressures—around 100 kPa, comparable to everyday atmospheric pressure. This suggests that the method is both safe and practical for clinical applications. Additionally, the researchers validated their observations using theoretical models, confirming that microjets are the primary factor in cell membrane perforation.
“This discovery not only provides a clearer understanding of how microbubbles interact with cells but also paves the way for optimizing ultrasound parameters to maximize drug delivery efficiency while minimizing patient risk,” said Supponen. Further refinements in microbubble coatings and ultrasound frequencies could enhance the precision of this technique, making it a powerful tool in targeted therapies.
A New Frontier in Medicine
By elucidating the physical principles behind microbubble-mediated drug delivery, the ETH Zurich team has set the stage for more effective and safer treatments for brain diseases and other conditions requiring targeted drug administration. Their work highlights the potential of physics-driven approaches in advancing medical therapies and improving patient outcomes.
Disclaimer:
This article is based on research findings and does not constitute medical advice. The microbubble drug delivery technique is still under investigation and has not yet been approved for clinical use. Patients should consult their healthcare providers for information on currently available treatment options.
Source: ETH Zurich
Journal Reference: Cattaneo, M., et al. (2025). Cyclic jetting enables microbubble-mediated drug delivery. Nature Physics. doi.org/10.1038/s41567-025-02785-0.