Copenhagen, Denmark – February 23, 2025 – A groundbreaking study by researchers at the University of Copenhagen and the Max Planck Institute of Biochemistry has unveiled how genetic factors influence blood protein levels during childhood and adolescence. This research, published in Nature Genetics, lays the foundation for understanding disease mechanisms and developing improved diagnostic tools.
Key Findings from the Study
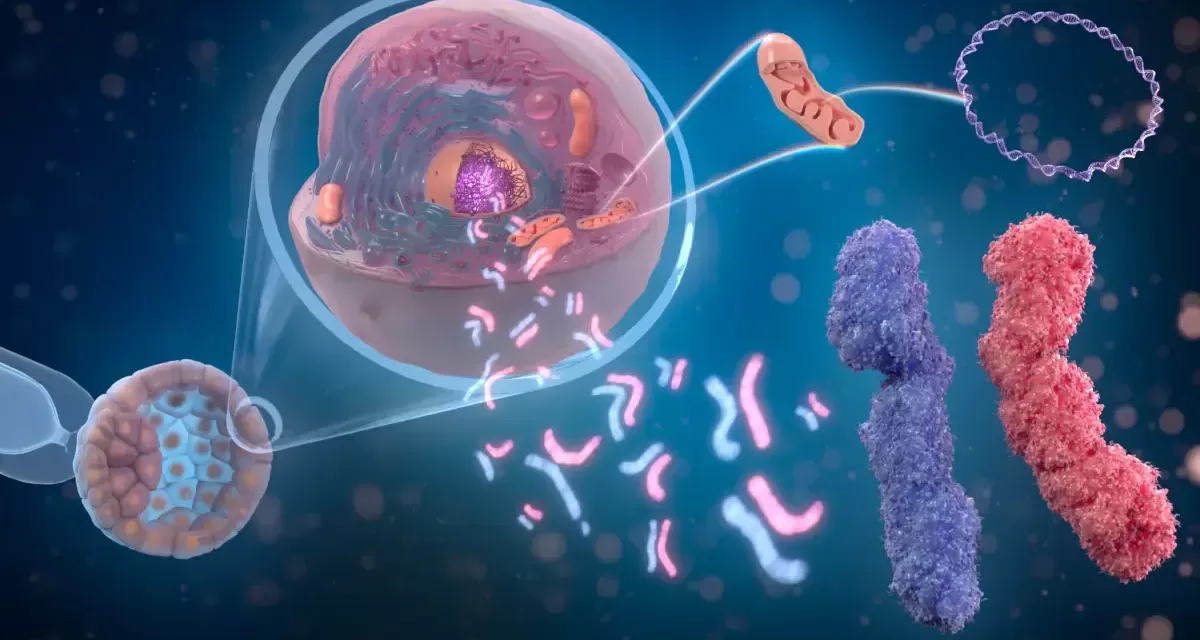
A large-scale study involving over 3,000 Danish children and adolescents has provided new insights into how blood proteins evolve during pediatric development. Led by Professor Matthias Mann at the Max Planck Institute of Biochemistry and Professors Torben Hansen and Simon Rasmussen at the University of Copenhagen, the study leveraged advanced mass spectrometry to analyze more than 1,200 different proteins in blood samples from individuals aged 5 to 20 years.
The findings indicate that 70% of these proteins are influenced by various factors, including age, sex, body mass index (BMI), and genetic variants. “Plasma protein levels are influenced by various factors, but their impact varies from protein to protein. By breaking down the sources of variation, we found that some proteins are primarily driven by genetics, while others are more affected by age or obesity,” explained Dr. Lili Niu, the study’s first author.
Genetic Influence and Puberty Differences
One of the most striking discoveries was the impact of genetic variants on protein levels, with some variants causing up to 30-fold differences between individuals. The study also revealed significant sex-specific differences in protein trajectories during puberty, offering clues as to why males and females experience different developmental patterns and disease susceptibilities.
“The genetic regulation of blood proteins provides insight into why children develop differently and why some are more prone to diseases than others,” said Professor Hansen.
Implications for Disease Research and Drug Development
Utilizing advanced statistical methods, the researchers identified 41 genes linked to 33 traits associated with heart disease and metabolism. “By connecting genes to proteins to disease, our findings open new avenues for understanding disease mechanisms and identifying potential drug targets,” noted Professor Rasmussen.
To further scientific collaboration, the team has launched an interactive web portal, proteomevariation.org, where researchers worldwide can explore how specific proteins change throughout childhood and adolescence.
“This study demonstrates how mass spectrometry-based proteomics is emerging as a powerful tool for large-scale population studies,” concluded Professor Mann. “With just a small drop of blood, we can measure thousands of proteins with unprecedented precision, paving the way for early disease detection and precision medicine.”
Future Directions
The researchers are now exploring whether these protein patterns can predict which children may develop certain diseases and how treatments can be tailored to individual needs. This comprehensive map of protein changes marks a significant step toward integrating proteomics into precision medicine.
Disclaimer: This article is based on findings published in Nature Genetics and aims to provide general information on the study. It is not intended to replace professional medical advice or guidance. For specific health concerns, consult a qualified healthcare professional.