A groundbreaking study has shed new light on why only 20% of advanced bladder cancer patients respond to immunotherapy. Led by the Biomedical Informatics Research Programme (GRIB) and the Cancer Programme at the Hospital del Mar Research Institute, in collaboration with Pompeu Fabra University, the research identifies key factors that influence treatment success or failure.
The study, published in Nature Communications, was coordinated by Mar Albà, Júila Perera, Joaquim Bellmunt, and Robert Castelo from the Department of Medicine and Life Sciences (MELIS) at UPF. By analyzing public data from over 700 patients across six different cohorts, the researchers aimed to uncover what differentiates responders from non-responders.
Tumor Subtypes and Treatment Response
One of the most striking findings of the study is that among the five recognized tumor subtypes in bladder cancer, the rarest one—the neuronal subtype—responds most favorably to immunotherapy. Other subtypes show significantly lower response rates.
GRIB researcher Lilian Marie Boll explained, “We found that for some patients, currently known markers effectively predict treatment response. However, for many others, additional biological factors likely play a role, necessitating further research.”
Key Markers for Immunotherapy Response
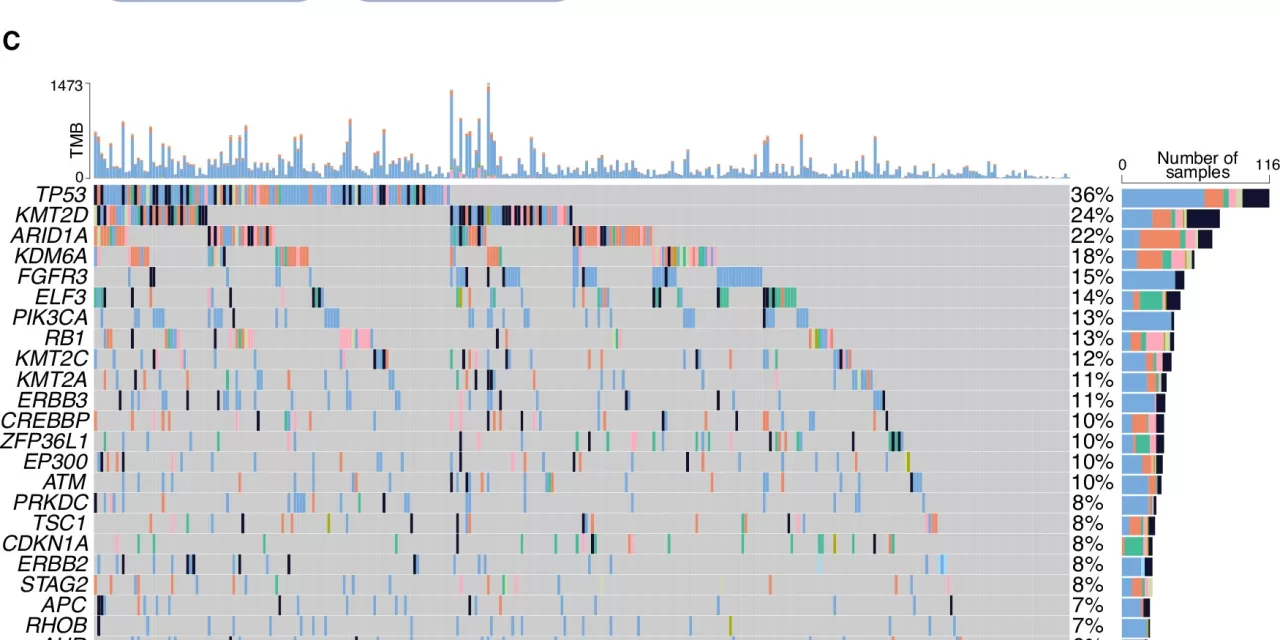
The research team developed a machine-learning algorithm to predict patient responses based on various tumor subtypes. Some of the most reliable markers include:
- Tumor Mutational Burden (TMB): The number of mutations present in the tumor.
- APOBEC Enzyme Mutations: These mutations are linked to tumor heterogeneity and affect how the immune system recognizes cancer cells.
- Proinflammatory Macrophages: The presence of these immune cells is associated with better treatment outcomes.
Additionally, the study identified certain markers in the tumor microenvironment that hinder immunotherapy effectiveness. The large dataset allowed researchers to pinpoint rare mutations that might help the immune system detect tumors more efficiently.
A New Approach to Patient Classification
Dr. Perera Bel, a GRIB researcher, highlighted that immune cell infiltration in tumors is an important factor but not a definitive predictor of treatment response. The study found that distinguishing between patients with and without immune infiltration improved the algorithm’s accuracy, suggesting that different sets of markers should be prioritized for each group.
Toward Precision Medicine
Dr. Bellmunt, coordinator of the Urologic Cancer Research Group at the Hospital del Mar Research Institute and the Dana-Farber Cancer Institute, emphasized that the study enhances understanding of tumor heterogeneity, a major challenge in immunotherapy. “Identifying immune cell populations that facilitate or inhibit immunotherapy response is crucial for improving treatment strategies,” he said.
The study underscores the necessity of large datasets for developing predictive models that can refine patient classification and enhance treatment personalization. By integrating extensive data, researchers hope to pave the way for more effective precision medicine approaches for bladder cancer and potentially other cancer types.
For more information, refer to the original study: Lilian Marie Boll et al, Predicting immunotherapy response of advanced bladder cancer through a meta-analysis of six independent cohorts, Nature Communications (2025). DOI: 10.1038/s41467-025-56462-0
Disclaimer:
This article is for informational purposes only and does not constitute medical advice. Patients should consult healthcare professionals for diagnosis and treatment decisions.