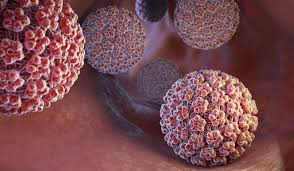
A groundbreaking study from the University of Michigan has found that self-sampling for human papillomavirus (HPV) screening is just as effective as traditional speculum-based exams. The findings, published in Preventive Medicine Reports and JAMA Network Open, could lead to significant changes in cervical cancer screening practices across the United States.
HPV is the most common sexually transmitted infection in the U.S. and is responsible for more than 99% of cervical cancer cases. Current screening methods require a speculum-based exam, which many patients find uncomfortable, especially those with physical disabilities.
Research Supports Self-Sampling
The University of Michigan researchers conducted two studies to compare the effectiveness of self-sampling with speculum-based testing. One study involved 193 participants between the ages of 25 and 65, who were either undergoing routine screening or at risk for cervical cancer. Participants provided vaginal swab samples, which were then tested for 15 high-risk HPV types. The study found that self-sampling provided results equivalent to traditional collection methods.
“We found that using swabs is equivalent to speculum-based collection,” said Dr. Diane Harper, senior author of both studies and professor of obstetrics and gynecology.
The research aligns with global data from countries such as Sweden, Australia, and the Netherlands, which have implemented self-sampling and experienced a reduction in cervical cancer incidence.
Improved Screening Access for Women with Disabilities
Another key aspect of the study focused on women with physical disabilities, a group that has historically faced significant barriers to cervical cancer screening. A separate study examined 56 women with disabilities and found that self-sampling was not only effective but also preferred over speculum exams.
“Women with physical disabilities have lower rates of cervical cancer screening due to multiple barriers, including inaccessible healthcare facilities and difficulty with positioning for a speculum exam,” said Dr. Susan Ernst, a clinical associate professor of obstetrics and gynecology and co-author of the study.
Participants described traditional speculum exams as “cold,” “traumatizing,” and “invasive.” In contrast, they found self-sampling to be “simple,” “comfortable,” and “feasible.”
“The swabs cannot replace having a conversation with your doctor. However, it can save the vast majority of women from getting unnecessary speculum tests,” Harper emphasized.
Future Implications for HPV Screening
Currently, cervical cancer screening and HPV testing are recommended for women every 3 to 5 years starting at age 25. However, researchers hope their findings will influence national guidelines to make self-sampling a widely accepted alternative to speculum exams. The team is working with U-M Health to integrate self-sampling as a primary screening method in their clinics.
“This is a great example of how multiple disciplines at Michigan Medicine work together,” Harper said. “Our next goal is to find a cure for HPV.”
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Readers should consult their healthcare providers for personalized recommendations regarding HPV screening and cervical cancer prevention.