A growing number of women experience high blood sugar levels during pregnancy, a condition known as gestational diabetes. While these levels typically return to normal after birth, the long-term health risks for these mothers are significant, necessitating better screening and ongoing care.
The Prevalence and Risks of Gestational Diabetes
Gestational diabetes is the most common metabolic disorder in pregnancy, affecting one in seven women worldwide and one in sixteen in New Zealand. It is associated with several complications, including high blood pressure, increased birth weight of babies (leading to delivery complications), and higher rates of Cesarean sections. Additionally, it has a significant impact on the mother’s mental health and overall well-being.
Alarmingly, the number of women diagnosed with gestational diabetes continues to rise. A recent review of the long-term health effects of this condition suggests that postpartum care for these women can be significantly improved.
Long-Term Health Risks and the Need for Continued Care
Women who experience gestational diabetes are at a much higher risk of developing type 2 diabetes—ten times more likely than those who do not have the condition during pregnancy. Additionally, they face twice the risk of developing cardiovascular disorders such as heart disease. Mental health issues, including depression, are also more prevalent among these women, particularly among high-risk groups such as those of non-European ethnicity and those with a history of gestational diabetes.
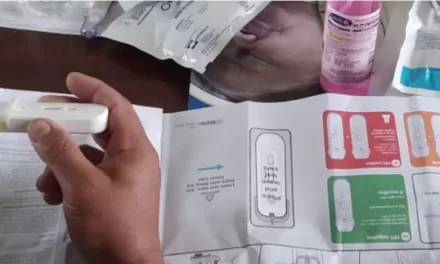
To mitigate these risks, ongoing care and regular health screenings after birth are crucial. This should include monitoring blood sugar levels, checking for cardiovascular issues, and assessing mental well-being. Equally important are dietary and exercise guidance, as well as support for continued breastfeeding. Women with gestational diabetes may experience delayed milk flow and lower breastfeeding rates, yet breastfeeding has been shown to reduce the risk of developing type 2 diabetes.
Experts recommend that screening should extend beyond the first year postpartum. However, many women do not receive adequate follow-up care. A 2018 British study found that women who had gestational diabetes felt abandoned by the healthcare system after giving birth. Similarly, a 2024 New Zealand study revealed that mothers who had gestational diabetes still needed more support from the healthcare system years after giving birth.
Gaps in Clinical Guidelines and Future Improvements
A research team recently reviewed clinical practice guidelines from 22 countries, including New Zealand, and found significant gaps in postnatal care recommendations for women who had gestational diabetes.
One major concern is the lack of postnatal diabetes screening. While it is standard practice to test women’s blood sugar levels within three months after birth, only about half of New Zealand women receive this screening within six months postpartum. Encouraging attendance through reminder systems or combining tests with routine baby health check-ups could improve these numbers. However, very few existing guidelines provide recommendations on how to enhance screening rates.
Another gap is mental health screening. Despite the increased likelihood of postpartum depression and anxiety among women with a history of gestational diabetes, guidelines rarely include recommendations for psychological assessments. A 2022 study found that one in five women with previous gestational diabetes reported symptoms of anxiety, depression, or poor mental functioning six months after giving birth. Experts advocate for routine mental health screenings for these women to improve postnatal care.
Healthcare professionals play a crucial role in supporting women with a history of gestational diabetes. Counseling on long-term health risks, encouraging screening attendance, and promoting healthy lifestyle choices can significantly impact these women’s well-being and reduce the likelihood of developing serious conditions like type 2 diabetes and heart disease.
Conclusion
Gestational diabetes poses significant risks to mothers long after childbirth, yet postnatal care often falls short of recommended standards. Improved clinical guidelines, increased awareness, and proactive healthcare interventions are necessary to provide better support for these women. By prioritizing long-term screening and mental health care, the medical community can help mitigate the risks associated with gestational diabetes and improve outcomes for affected mothers.
Disclaimer: This article is based on research and expert reviews but should not be considered medical advice. Women who have had gestational diabetes should consult their healthcare provider for personalized recommendations and follow-up care.