Mitochondria, the powerhouses of the cell, play a crucial role in energy production and cellular function. However, new research suggests that mitochondrial dysfunction may be a key factor in the development of type 2 diabetes, raising the possibility that reversing such damage could offer a potential cure.
A recent study published in Science by researchers at the University of Michigan has found that mitochondrial defects in insulin-producing pancreatic β-cells can trigger a stress response that impairs their ability to produce insulin. Since type 2 diabetes is characterized by the body’s inability to produce or effectively use insulin, this discovery could pave the way for new therapeutic strategies.
Unraveling the Mystery of Mitochondrial Dysfunction
Scientists have long known that diabetic patients’ β-cells have abnormal mitochondria, but the reasons behind this phenomenon remained unclear. To investigate, the research team led by Emily M. Walker, Ph.D., a research assistant professor of internal medicine, deliberately damaged three key components of mitochondrial function in mice.
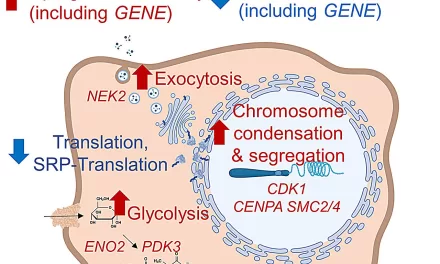
“In all three cases, the exact same stress response was activated,” Walker explained. “This response caused β-cells to become immature, cease insulin production, and essentially stop functioning as β-cells.”
The team also confirmed their findings in human pancreatic islet cells, strengthening the evidence that mitochondrial dysfunction plays a central role in diabetes.
Mitochondrial Dysfunction Beyond β-Cells
Given that diabetes affects multiple organs and tissues, the researchers expanded their investigation to other cell types, including liver and fat-storing cells. They found that the same stress response was triggered in these cells, leading to functional impairments.
“Diabetes is a multi-system disease,” said Scott A. Soleimanpour, M.D., director of the Michigan Diabetes Research Center and senior author of the study. “Since we observed the same mitochondrial stress response in different tissues, we believe this mechanism could be widespread in diabetes-related dysfunction.”
A Potential Path to Reversal
Despite the damage, the affected cells did not die—a crucial finding that opened the door to potential therapeutic interventions. The researchers tested a drug called ISRIB, which blocks the stress response, and observed promising results. Within four weeks of treatment, β-cells in mice regained their ability to control glucose levels.
“Losing β-cells is one of the main pathways to developing type 2 diabetes,” Soleimanpour noted. “Our findings not only explain what may be happening at the cellular level but also suggest a way to intervene and potentially reverse the disease.”
The team is now focusing on further dissecting the disrupted cellular pathways and testing their approach in human diabetic cell samples. If successful, this research could mark a breakthrough in diabetes treatment.
Disclaimer
This article is based on scientific research and is intended for informational purposes only. The findings discussed are preliminary, and further studies are required before any clinical applications can be confirmed. Individuals should consult healthcare professionals before considering any new treatments.