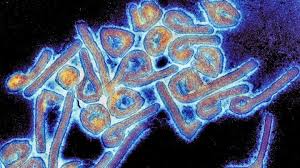
Kigali, Rwanda – July 2024: Rwanda faced its first-ever outbreak of the deadly Marburg virus in July 2024, challenging the nation’s healthcare infrastructure. However, a swift and coordinated response helped limit fatalities and prevent wider transmission, demonstrating Rwanda’s robust health system and pandemic preparedness.
The outbreak, originating in a referral hospital in Kigali, prompted health authorities to rethink traditional epidemic control measures. Unlike conventional assumptions that outbreaks start in rural areas, this incident highlighted the importance of rapid detection and containment regardless of location.
A Race Against Time
Health Minister Sabin Nsanzimana was attending the UN General Assembly in New York when he received an urgent message about the outbreak. Initially in disbelief, confirmation soon followed, setting off a national emergency response.
“We need to build the capacity to detect and contain an outbreak wherever it emerges,” Nsanzimana emphasized, advocating for a shift in epidemic response strategies.
Rwanda’s rapid deployment of scientific research and streamlined bureaucratic coordination proved critical. The country achieved the lowest-ever recorded fatality rate for Marburg at 23%, well below the disease’s average mortality rate of 50%.
Scientific and Medical Breakthroughs
Of the 66 confirmed cases, 51 patients recovered, with no new infections reported after 42 consecutive days, according to the Rwanda Biomedical Center (RBC). The outbreak claimed 15 lives, most of whom were experienced healthcare professionals.
Key to Rwanda’s success was the swift acquisition of investigational vaccines and medical supplies. The Sabin Vaccine Institute delivered 2,700 doses of trial vaccines for targeted clinical testing, offering hope for future treatment solutions.
Yvan Butera, Rwanda’s Minister of State for Health, highlighted the significance of genomic sequencing in containing the virus. “We found that our strain had a common ancestor with a 2014 outbreak, and it originated from bats in mining areas,” he explained.
Leadership and Global Cooperation
A dedicated command post was established to oversee the crisis response, integrating multiple sectors, including health, local governance, and security.
“What made it work was how quickly people could act. We cut bureaucracy, made decisions fast, and had everyone’s support,” said Annick Ishimwe, division manager of medical technology.
International partners played a crucial role, with support arriving within 24 hours of the first confirmed case. WHO Representative Brian Chirombo praised Rwanda’s response, stating, “Committed leadership, strong health systems, and global solidarity are key in tackling public health emergencies.”
Looking Ahead
While Rwanda successfully contained the Marburg outbreak, neighboring Tanzania is now facing its second wave, with a confirmed case in Kagera. The continued spread of the virus underscores the need for sustained vigilance, research, and global collaboration.
Although no approved vaccines or antiviral treatments currently exist for Marburg, Rwanda’s response serves as a model for outbreak management. Lessons learned from Kigali’s containment efforts could inform future strategies in combating infectious diseases worldwide.
As Rwanda moves forward, health authorities remain focused on strengthening surveillance, enhancing medical research, and fostering global partnerships to ensure rapid responses to future health crises.
Disclaimer: This article is based on information provided by SciDev.Net and official sources. While efforts have been made to ensure accuracy, new developments or updates may alter certain details. Readers are encouraged to refer to official health agencies for the most current information.