New research highlights the role of low-dose antibiotic exposure in accelerating antimicrobial resistance.
A recent study by researchers at the John Innes Centre has shed light on how bacteria develop resistance to multiple drugs, furthering our understanding of antimicrobial resistance—one of the top threats to global public health. The findings, published in the journal Antimicrobial Agents and Chemotherapy, emphasize the dangers of antibiotic misuse and the urgent need for responsible antibiotic stewardship.
Understanding the Resistance Mechanism
The study, led by Professor Tony Maxwell, explored earlier research suggesting that exposure to low doses of quinolone antibiotics could lead to bacteria developing resistance to other unrelated antibiotics. Quinolones are widely used antibiotics that target DNA gyrase, an enzyme crucial to bacterial survival. The ability of bacteria to evolve resistance mechanisms against such antibiotics poses a significant challenge in medical and agricultural settings.
Experiment and Findings
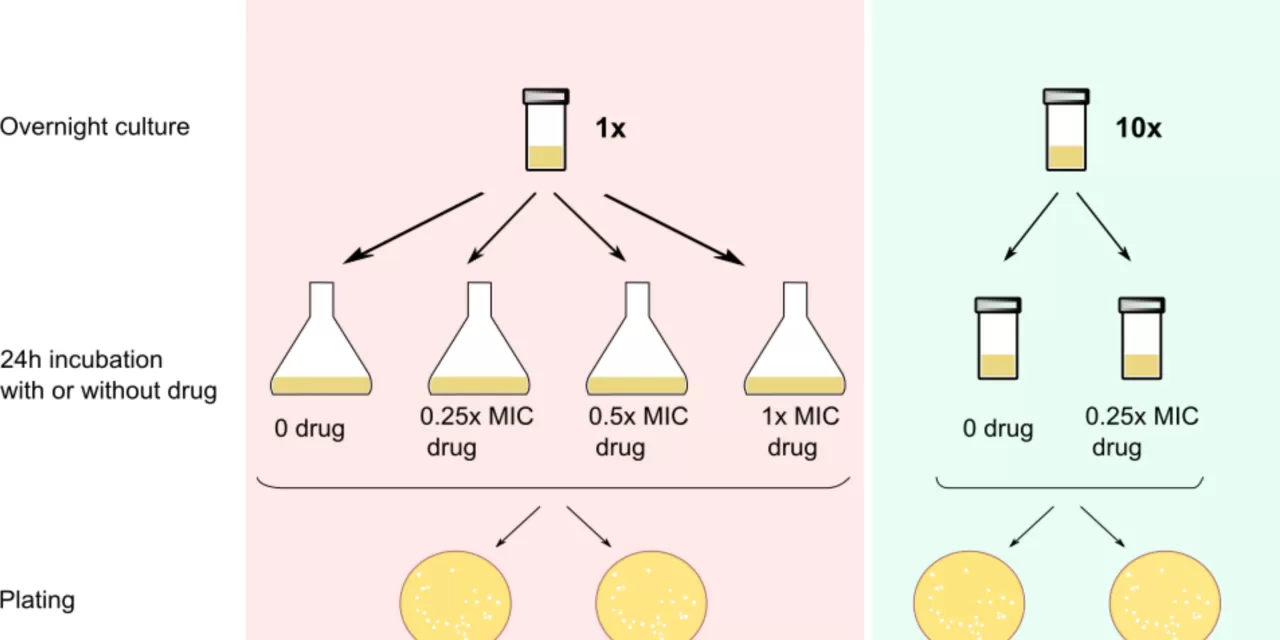
The research team conducted experiments using Escherichia coli (E. coli) bacteria exposed to non-lethal concentrations of four types of quinolones: ciprofloxacin, moxifloxacin, oxolinic acid, and norfloxacin. The bacterial colonies were then tested against non-quinolone antibiotics to assess their survival rates.
The results revealed that all tested quinolones except moxifloxacin contributed to Quinolone-Induced Antibiotic Resistance (QIAR). Whole genome sequencing of the bacteria indicated that resistance stemmed from various mutations in the bacterial DNA induced by quinolone exposure. The findings also suggested that moxifloxacin might kill E. coli through a different mechanism compared to other quinolones.
Implications for Medicine and Agriculture
Professor Maxwell emphasized the importance of avoiding exposure to low doses of quinolones, as this can contribute to the development of drug-resistant bacteria. He noted that such exposure could result from improper use in human medicine, agricultural practices, or pharmaceutical industry contamination of the environment.
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi, and parasites evolve to resist the drugs designed to eliminate them. While AMR is a natural process, it has been drastically accelerated by the overuse and misuse of antibiotics in healthcare and agriculture. Without urgent intervention, AMR could lead to an estimated 10 million deaths per year and cost the global economy up to 10 trillion USD annually by 2050.
The World Health Organization has identified antibiotic stewardship and the development of new antibiotics as critical strategies to combat this growing threat.
Call for Action
The study underscores the need for stricter regulations on antibiotic use and increased public awareness regarding the dangers of self-medication and incomplete antibiotic courses. Reducing environmental contamination from pharmaceutical waste and promoting research into alternative treatments are also essential steps in addressing antimicrobial resistance.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult a healthcare professional before taking or discontinuing any medication.
For more information: Natassja G. Bush et al., “Insights into antibiotic resistance promoted by quinolone exposure,” Antimicrobial Agents and Chemotherapy (2024). DOI: 10.1128/aac.00997-24.