A groundbreaking study published in Pediatric Research sheds new light on the relationship between two significant neonatal brain injuries—neonatal hypoxic-ischemic encephalopathy (HIE) and perinatal arterial ischemic stroke (PAIS). Both of these conditions are major contributors to infant death and long-term disabilities, and the new findings could help improve diagnosis and treatment strategies.
HIE, which affects one to three in 1,000 live births per year, results from a global reduction of blood flow and oxygen to the brain. It accounts for approximately 22% of all infant deaths worldwide. PAIS, while slightly less common, is caused by a clot obstructing the flow of blood to a major brain artery. These two conditions can lead to serious brain damage, seizures, and neurological and developmental complications that persist into later childhood.
While researchers have long understood that HIE and PAIS are different in terms of their mechanisms, a new study set out to explore how often they occur together in neonates. Led by Dr. Jessica Wisnowski and her colleagues from several U.S. pediatric hospitals, the study analyzed data from 473 infants with moderate to severe HIE enrolled in the HEAL Trial. These infants, who underwent brain MRIs within six hours of birth, were assessed for the presence of PAIS and its potential correlation with various clinical outcomes.
The study uncovered the following key findings:
- 4% of infants with moderate to severe HIE also showed MRI evidence of PAIS.
- Of those with PAIS, three out of four also displayed an HIE-pattern brain injury and faced more severe complications than those without PAIS.
- Seizures were significantly more common in infants with both conditions.
- Infants with PAIS were more likely to experience persistent encephalopathy five days into treatment compared to those without PAIS.
Despite these findings, the study was limited by the small sample size of infants with both HIE and PAIS, which prevented researchers from drawing statistically significant conclusions about two-year neurodevelopmental outcomes.
Researchers speculate that several factors could explain the overlap between HIE and PAIS. Shared risk factors, such as chorioamnionitis and placental disease, may contribute to both conditions. Additionally, treatments for HIE, including extracorporeal membrane oxygenation (ECMO), may increase the risk of stroke, which is more prevalent in infants with PAIS. Furthermore, the occurrence of PAIS during labor could lead to prolonged deliveries, increasing the risk of HIE.
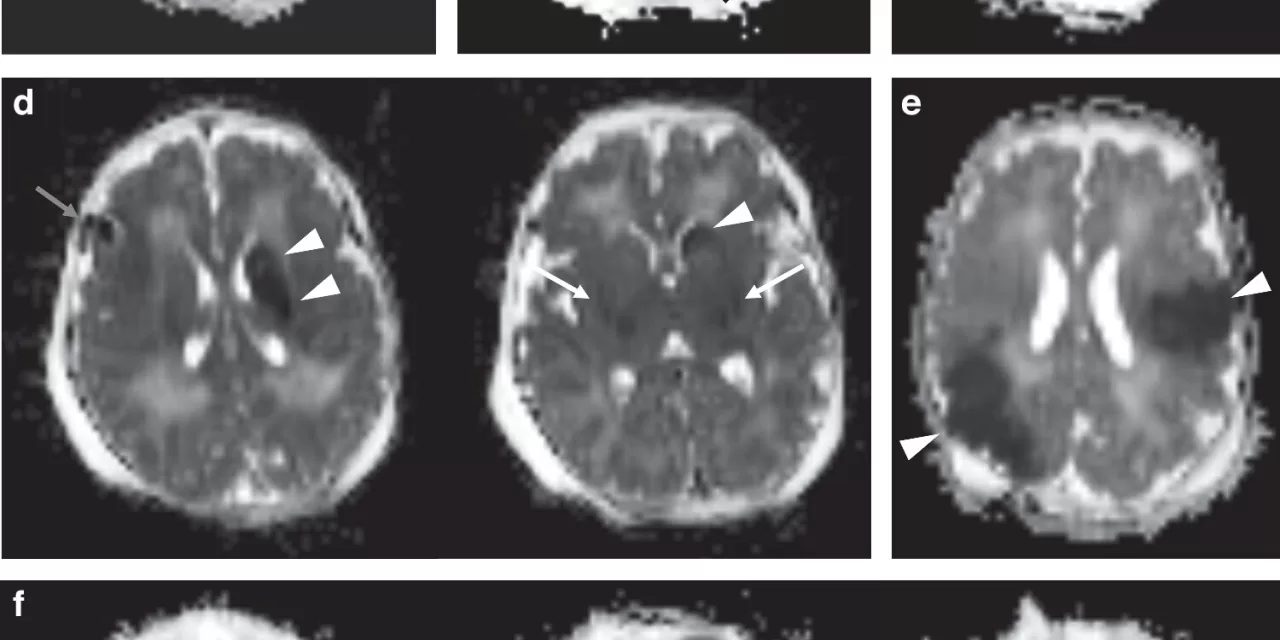
The study highlights the importance of comprehensive brain MRI scans in diagnosing and understanding neonatal brain injuries. “This study emphasizes the importance of brain MRI in identifying all causes of brain injury in infants undergoing therapeutic hypothermia for HIE,” says Dr. Wisnowski. “We hope that this research helps guide diagnosis and treatment advances for these leading causes of infant death and long-term disability.”
While significant strides have been made in identifying the overlap between HIE and PAIS, more research is necessary to further understand the timing and pathogenesis of these conditions. The study’s authors emphasize that large-scale studies are critical in improving interventions for neonatal brain injury, potentially leading to better outcomes for affected infants.
Disclaimer: This article is based on research findings and is for informational purposes only. Always consult a healthcare professional for advice related to medical conditions and treatments.