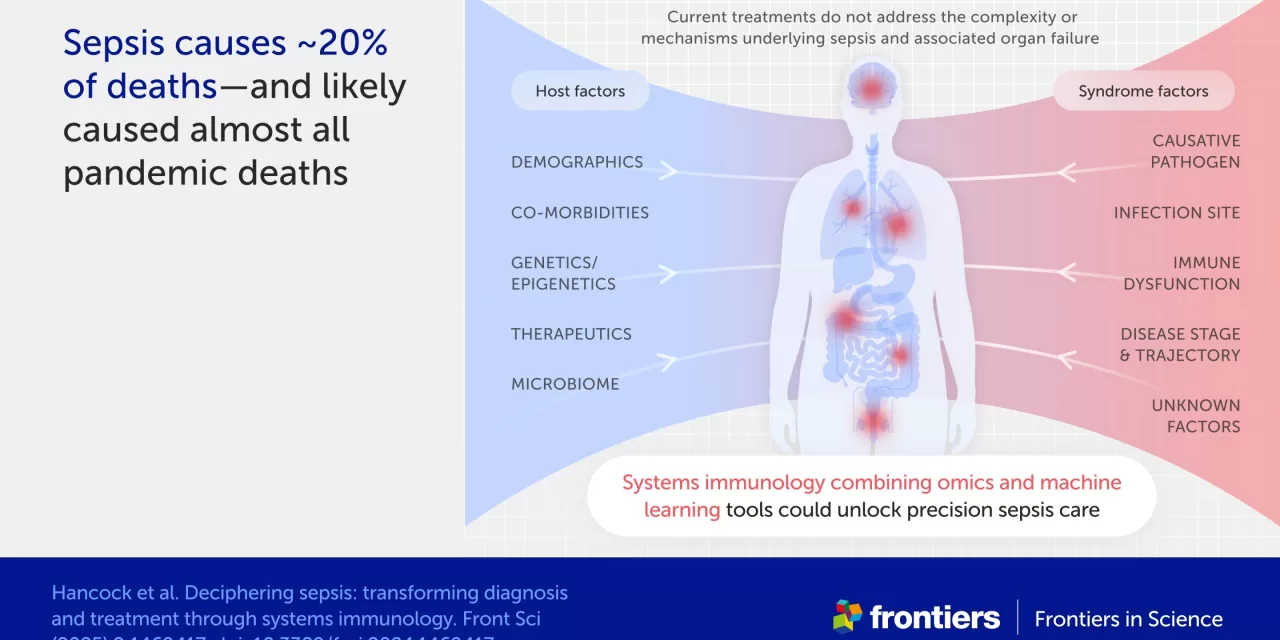
Sepsis remains one of the most underestimated yet deadly medical conditions, accounting for approximately 20% of global deaths. Nearly a quarter of hospitalized sepsis patients do not survive, primarily because sepsis is not often recognized as a direct cause of death due to its complex nature. Despite its staggering mortality rate, no targeted treatments currently exist to combat sepsis effectively.
However, a new study published in Frontiers in Science highlights the potential of systems immunology in understanding and treating sepsis. This advancement could significantly cut the death toll in future pandemics, irrespective of the disease that triggers them.
The Need for a Unified Approach
Professor Robert Hancock from the University of British Columbia, the lead author of the study, emphasizes the need for greater investment in sepsis research.
“We need to adopt a concerted approach to tackle sepsis,” Hancock stated. “Only a very small amount of funding is currently invested in sepsis research and product development—yet sepsis is as prominent a cause of death as heart disease and cancer, and the major cause of death in pandemics.”
Systems Immunology and Precision Medicine
One of the biggest challenges in diagnosing and treating sepsis is its complexity. Sepsis occurs when an infection leads to immune system failure, causing multi-organ dysfunction. Because sepsis can arise from a wide range of infections, its symptoms vary widely among patients, making early detection difficult. This delay in diagnosis contributes significantly to high mortality rates.
Systems immunology offers a promising solution by integrating mathematical and computational modeling to analyze how the immune system interacts with the body’s other systems. Using clustering analysis, researchers can identify patterns in large volumes of biological data—such as transcriptomics (gene expression changes), proteomics, and metabolomics—providing detailed insights into the body’s response to sepsis.
Through this approach, scientists have already identified genetic markers that serve as early warnings for sepsis. They have also classified five distinct sepsis subtypes, each with unique immune dysregulation patterns and prognoses. In the future, these insights could pave the way for earlier diagnosis and more effective, personalized treatment plans.
Challenges in Implementation
Despite its potential, systems immunology is not yet widely used in sepsis treatment. The main barriers are the high costs and the vast amounts of data required for meaningful analysis. Hancock and his team urge for increased funding and data availability to advance this field.
“In sepsis, we lack the depth of information required to enable more effective systems immunology and machine learning approaches,” Hancock explained. “We hope to encourage the development of large, in-depth patient studies that will generate new insights.”
The Role of Sepsis in Past and Future Pandemics
Effectively treating sepsis could be a game-changer in pandemic preparedness. Viral sepsis was a major cause of death in severe COVID-19 cases, and historical pandemics such as the 1918 influenza pandemic and the bubonic plague also saw high mortality due to sepsis-related complications.
By tackling sepsis, medical professionals could significantly reduce death rates in future pandemics, regardless of the infection responsible. Moreover, since sepsis-related immune dysfunction can persist long-term—leading to conditions similar to post-viral syndromes like long COVID—advancing sepsis treatment could also benefit those suffering from chronic illnesses.
A Call for Greater Investment
The study underscores the urgent need for increased funding and larger-scale research. Systems immunology methods, such as omics-based analyses, are costly per patient, making widespread implementation challenging. Researchers emphasize the importance of collaboration among stakeholders to generate the necessary data for further discoveries.
“We need to invest in larger omics studies, develop new animal and organoid models that reflect sepsis heterogeneity, and advance early diagnostics and immune-targeted treatments,” Hancock concluded.
With a focused and well-funded effort, tackling sepsis could not only save millions of lives annually but also fortify global health systems against future pandemics.
Disclaimer: This article is for informational purposes only and is based on current scientific research. It should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider regarding any medical concerns.