A recent study highlights the growing benefits of HPV self-sampling kits in making cervical cancer screening more accessible, comfortable, and empowering for women, especially those who have historically faced barriers in accessing healthcare. The study, published in Current Oncology, finds that self-sampling kits offer a more convenient, private, and less traumatic alternative to traditional Pap tests, empowering individuals with more control over their reproductive health.
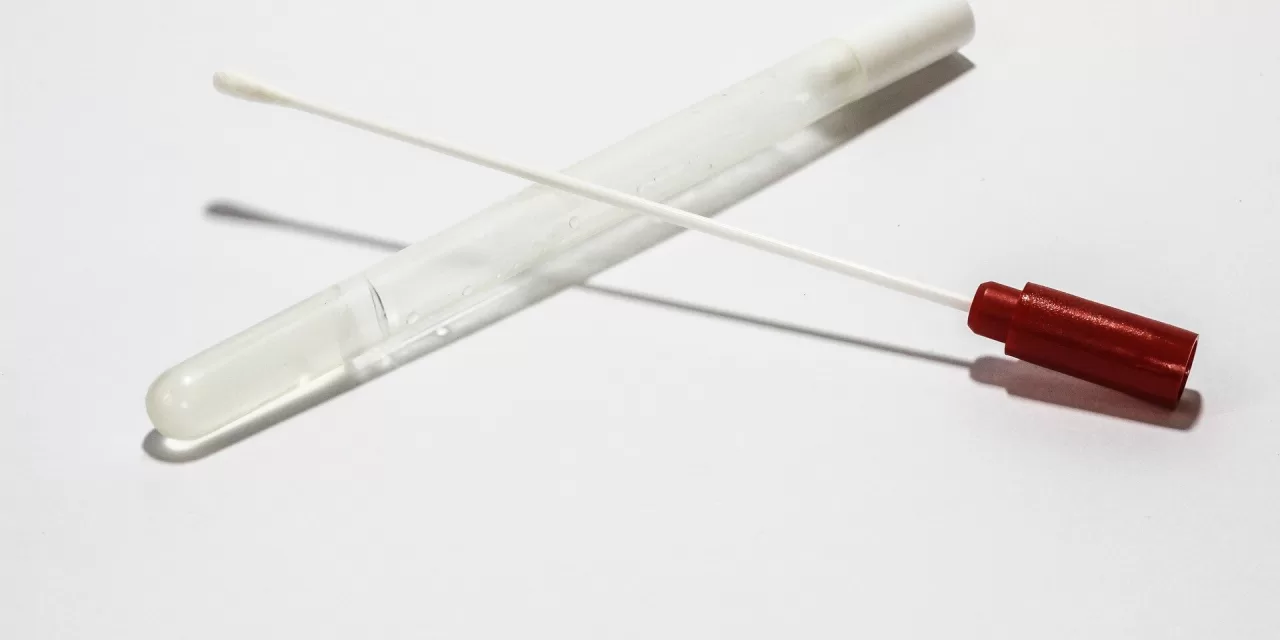
According to the study’s lead author, Mandana Vahabi, the women’s health research chair at Unity Health Toronto, and a professor at the University of Toronto’s Lawrence Bloomberg Faculty of Nursing, self-sampling kits are as simple to use as at-home COVID tests. “With this method, individuals can test themselves at a time and place that is convenient for them,” Vahabi says. “The self-insertion of the swab is less uncomfortable than traditional methods, providing a more comfortable experience for users.”
For many individuals, especially those from marginalized groups such as sex workers, formerly incarcerated women, or those who have experienced sexual violence, the stigma and discomfort associated with traditional screening methods often discourage participation in cervical cancer prevention. The study found that many participants had either never had a Pap test or avoided follow-up screenings due to fear of judgment, underscoring the importance of self-sampling as a viable option.
One of the significant findings of the study is that a third of participants tested positive for high-risk strains of HPV, which are linked to cervical cancer. These individuals were subsequently referred for follow-up testing, highlighting the critical role of early detection in preventing the progression of the disease. Early intervention options include treatments such as laser surgery, cryosurgery (freezing), or the removal of damaged tissue to prevent further health complications.
HPV, a virus with over 100 strains, includes four high-risk types that are most commonly associated with the development of cervical cancer. “HPV self-sampling is not just about convenience,” Vahabi emphasizes. “It’s about providing women with the tools they need to detect potential health issues early and access interventions that could save their lives.”
Vahabi is a strong advocate for the integration of HPV self-sampling into regular cervical cancer screening programs, noting the numerous structural barriers women face in accessing traditional screenings, including the lack of primary care providers and social stigmas. “Our study showed how stressful it is for sex workers to seek screening because they face stigmatization and judgment about their occupation,” she explains. “This creates unnecessary fear and prevents them from seeking life-saving resources.”
While there are challenges in scaling up HPV self-sampling, such as mistrust of healthcare providers and lack of confidence in using the test kits, Vahabi believes these can be addressed through educational tools, such as instructional videos, illustrated pamphlets, and access to nurse practitioners for guidance and support.
Despite the progress, public knowledge about HPV and cervical cancer remains limited. Vahabi advocates for more effective public education, explaining that HPV can affect anyone, regardless of the number of sexual partners, and that screening is vital for everyone. “We need to help people understand the importance of both vaccination and regular screenings to prevent the spread of the virus and its potential to cause cancer,” she says.
The study was published in Current Oncology in 2024, under the title “Breaking Barriers: Empowering Cervical Cancer Screening with HPV Self-Sampling for Sex Workers and Formerly Incarcerated Women in Toronto.”
Disclaimer: This article is based on the research conducted by Mandana Vahabi and her team, and the findings discussed represent the results of their study. Please consult with healthcare providers for professional medical advice.