Description of the situation
Introduction
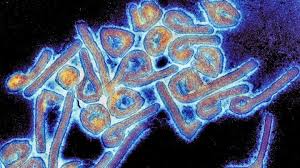
On 13 January 2025, WHO informed its Member States and IHR State Parties of an outbreak of suspected Marburg Virus Disease (MVD) in the Kagera region of the United Republic of Tanzania using our secure web-based platform—the Event Information Site (EIS). Under the International Health Regulations, the EIS is used to issue rapid alerts to Member States of acute and rapidly developing public health risks and events with possible international implications.
Summary of the situation
On 10 January 2025, WHO received reliable reports from in-country sources regarding suspected cases of MVD in the Kagera region of the United Republic of Tanzania. Six people were reported to have been affected, five of whom had died. The cases presented with similar symptoms of headache, high fever, back pain, diarrhoea, haematemesis (vomiting with blood), malaise (body weakness) and, at a later stage of disease, external haemorrhage (bleeding from orifices).
As of 11 January 2025, nine suspected cases were reported including eight deaths (case fatality ratio (CFR) of 89%) across two districts – Biharamulo and Muleba. Samples from two patients have been collected and tested by the National Public Health Laboratory. Results are pending official confirmation. Contacts, including healthcare workers, are reported to have been identified and under follow-up in both districts.
The Bukoba district in Kagera region experienced its first MVD outbreak in March 2023, and zoonotic reservoirs, such as fruit bats, remain endemic to the area. The outbreak in March 2023 lasted for nearly two months with nine cases including six deaths.
Public health response
National rapid response teams have been deployed to support outbreak investigation and response; surveillance activities have been intensified with contact tracing ongoing; laboratory samples from recent cases have been sent for confirmation at the National Public Health Laboratory. A mobile laboratory is located in Kagera region and treatment units have reportedly been established.
WHO risk assessment
The risk of this suspected MVD outbreak is assessed as high at the national level due to several concerning factors. The suspected outbreak thus far involves at least nine suspected cases, including eight deaths, resulting in a high CFR of 89%. Healthcare workers are included among the suspected cases affected, highlighting the risk of nosocomial transmission. The source of the outbreak is currently unknown.
The reporting of suspected MVD cases from two districts suggests geographic spread. The delayed detection and isolation of cases, coupled with ongoing contact tracing, indicates lack of a full information of the current outbreak. More cases are expected to be identified.
The regional risk is considered high due to Kagera region’s strategic location as a transit hub, with significant cross-border movement of the population to Rwanda, Uganda, Burundi and the Democratic Republic of the Congo. Reportedly, some of the suspected cases are in districts near international borders, highlighting the potential for spread into neighbouring countries. MVD is not easily transmissible (i.e. in most instances, it requires contact with the body fluids of a sick patient presenting with symptoms or with surfaces contaminated with these fluids). However, it cannot be excluded that a person exposed to the virus may be travelling.
The global risk is currently assessed as low. There is no confirmed international spread at this stage, although there are concerns about potential risks. Kagera region, while not close to Tanzania’s capital or major international airports, is well-connected through transportation networks, and has an airport that connects to Dar es Salaam for onward travel outside Tanzania by air. This highlights the need for enhanced surveillance and case management capacities at relevant points of entry and borders, and close coordination with neighbouring countries to strengthen readiness capacities.
WHO advice
Human-to-human transmission of Marburg virus is primarily associated with direct contact with the blood and/or other bodily fluids of infected people. WHO advises the following risk reduction measures be taken as an effective way to reduce MVD transmission and control an outbreak.
Prevention: Protective measures individuals should take to reduce human exposure to the virus include:
- Reduce the risk of human-to-human transmission in the community arising from direct or close contact with infected patients, particularly with their body fluids. Close physical contact with MVD patients should be avoided.
- People suspected or confirmed for MVD should immediately seek care in health facilities and be isolated in a designated treatment centre for early care and to avoid transmission at home.
- Community and family members should avoid caring for symptomatic individuals at home, and avoid touching bodies of people deceased with MVD symptoms. They should avoid touching other potentially contaminated items and surfaces. They should be encouraged to go to a health facility for assessment and treatment if they have symptoms.
- Reduce the risk of bat-to-human transmission arising from prolonged exposure to mines or caves inhabited by fruit bat colonies. During work or research activities or tourist visits in mines or caves inhabited by fruit bat colonies, people should wear gloves and other appropriate protective clothing (including masks). During outbreaks, all animal products (blood and meat) should be thoroughly cooked before consumption.
Coordination: Multisectoral coordination and pillar meetings at all levels and sharing of detailed situation reports is encouraged. Involvement of different stakeholders and partners in preparedness and response activities is also encouraged. To ensure an effective and sustained response, resource mobilization efforts within the government and with partners are recommended.
Risk communication and community engagement: Raising public awareness and engaging with communities are important for successfully controlling MVD outbreaks. This includes raising awareness of symptoms, risk factors for infection, protective measures and the importance of seeking immediate care at a health facility. Sensitive and supportive information about safe and dignified burials is also crucial. This awareness should be increased through targeted campaigns and direct work with communities. Special attention should be given to high-risk groups, such as traditional healers, clergy, and community leaders, who may inadvertently facilitate disease spread, and who are important sources of information for the community. Misinformation and rumours should be addressed to foster trust and promote early symptom reporting.
Surveillance: Active case detection, contact tracing, and alert management across affected and neighbouring regions should be intensified. Community-based surveillance systems should be strengthened to promptly identify and report new cases, particularly in high-risk areas. Close monitoring of healthcare workers, family members and individuals who have had contact with suspected cases or other high-exposure settings should be ensured. Surveillance capacities should also be intensified at relevant points of entry and borders to reduce the risk of further spread, including internationally.
- Infection prevention and control (IPC) measures: critical infection prevention and control measures should be implemented and/or strengthened in all health care facilities, per WHO’s Infection prevention and control guideline for Ebola and Marburg disease, which highlighted the importance of the rapid implementation of the IPC ring approach including but not limited to IPC rapid assessment, decontamination of the health facilities and household and early detection and identification of the cases through the screening and isolation of the suspected cases to minimize the transmission risk.
- Health workers caring for patients with confirmed or suspected MVD should apply transmission-based precautions in addition to: standard precautions, including appropriate use of personal protective equipment (PPE) and hand hygiene according to the WHO 5 moments to avoid contact with patient’s blood and other body fluids and with contaminated surfaces and objects. Waste generated in healthcare facilities must be safely segregated, safely collected, transported, stored, treated and finally disposed. Follow the national guidelines, rules and regulations for safe waste disposal or follow the WHO’s guidelines on safe waste management
- Patient-care activities should be undertaken in a clean and hygienic environment that facilitates practices related to the prevention and control of health-care-associated infections (HAIs) as outlined in Essential environmental health standards in health care. Safe water, adequate sanitation and hygiene infrastructure and services should be provided in healthcare facilities. For details on recommendations and improvement, follow the WASH FIT implementation Package
Laboratory testing: The processing and analysis of samples should be expedited, with results promptly shared with responders and clinicians to guide patient management, containment strategies and broader response efforts. This includes genomic sequencing on positive samples. International referral of samples to a regional reference laboratory should be considered for inter-laboratory comparison.
Evaluation of candidate medical countermeasures: There are no licensed vaccines or therapeutics against MVD. Several candidate vaccines are in the pipeline and outbreaks offer an opportunity to assess their efficacy and safety. There are protocols available and a network of experts in filovirus ready to support national researchers.
Safe and dignified burials: Safe and dignified burial protocols should be implemented for people who have died to minimize community exposure. Additional training and equipment for healthcare workers and burial teams should be provided to ensure safe management of MVD-related fatalities. Thorough community engagement is required to ensure that affected communities are empowered to adhere to the protocol.
Case management and mental health and psychosocial support: Isolation and treatment facilities should be adequately equipped to ensure the safety and efficacy of patient care, while simultaneously preventing the spread of the disease. Supportive care such as rehydration, symptom management, and psychological support for patients and their families is essential to improving survival rates and mitigating the outbreak’s impact.
Border health and cross-border coordination: Surveillance and response capacities should be strengthened at relevant points of entry, onboard conveyances, and in border regions to prevent further spread, including internationally. Cases, contacts and individuals in affected areas who present signs and symptoms compatible with case definitions should be advised not to travel in line with WHO’s border health and points of entry technical guidance for filovirus disease outbreaks. Collaboration with neighbouring countries should be enhanced to harmonize reporting mechanisms, conduct joint investigations, and share critical data in real-time. Surrounding countries should enhance readiness activities to enable early case detection, isolation and treatment.
Preparedness and Readiness: Readiness assessments in high-risk regions should be conducted to ensure response mechanisms, such as mobile labs and isolation units, are adequately equipped to manage new cases.
Based on the current risk assessment, WHO advises against any travel and trade restrictions with the United Republic of Tanzania.
Further information
- WHO Factsheet- Marburg virus disease https://www.who.int/news-room/fact-sheets/detail/marburg-virus-disease
- Infection prevention and control guidelines for Ebola and Marburg disease, August 2023. https://www.who.int/publications/i/item/WHO-WPE-CRS-HCR-2023.1
- WHO Questions and Answers – Marburg virus disease.https://www.who.int/news-room/questions-and-answers/item/marburg-virus-disease Risk communication and community engagement for Marburg virus disease outbreaks. Interim Guidance November 2024. https://iris.who.int/bitstream/handle/10665/379761/B09185-eng.pdf?sequence=1
- Steps to putting on PPE for Ebola/Marburg coverall. https://www.who.int/multi-media/details/steps-to-put-on-ppe-for-ebola-marburg-disease-coverall
- Steps to removing PPE for Ebola/Marburg disease coverall. https://www.who.int/multi-media/details/steps-to-remove-ppe-for-ebola-marburg-disease-coverall
- Steps to putting on PPE for Ebola/Marburg gown and headcover. https://www.who.int/multi-media/details/steps-to-put-on-ppe-for-ebola-marburg-disease-gown-and-headcover
- Steps to removing PPE for Ebola/Marburg gown and headcover. https://www.who.int/multi-media/details/steps-to-remove-ppe-for-ebola-marburg-disease-gown-and-headcover
- Standard precautions for the prevention and control of infections: aide-memoire. https://www.who.int/publications/i/item/WHO-UHL-IHS-IPC-2022.1
- Transmission-based precautions for the prevention and control of infections: aide-memoire. https://www.who.int/publications/i/item/WHO-UHL-IHS-IPC-2022.2
- Essential environmental health standards in healthcare facilities- https://www.who.int/publications/i/item/9789241547239
- WASH FIT implementation for WASH improvements in healthcare facilities WASH FIT Fact Sheets | WASH in Health Care Facilities (washinhcf.org) https://www.washinhcf.org/wash-fit-fact-sheets/
- World Health Organization (March 2009). Hand hygiene technical reference manual: to be used by health-care workers, trainers and observers of hand hygiene practices. https://www.who.int/publications/i/item/9789241598606
- Ebola and Marburg diseases screening and treatment center design training. https://openwho.org/courses/ebola-marburg-screen-treat-facilities
- World Health Organization (2 June 2023). Disease Outbreak News; Marburg virus disease in the United Republic of Tanzania. https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON471
- Markotter W, Coertse J, DeVries M, et al. Bat-borne viruses in Africa: a critical review. J of Zoology. 2020;311:77-98. doi:10.1111/jzo.12769. https://zslpublications.onlinelibrary.wiley.com/doi/10.1111/jzo.12769(link is external)
- Korine C Rousettus aegyptiacus. The IUCN Red List of Threatened Species 2016: e.T29730A22043105. https://www.iucnredlist.org/species/29730/22043105
- Cross RW, Longini IM, Becker S, Bok K, Boucher D, Carroll MW, et al. (2022) An introduction to the Marburg virus vaccine consortium, MARVAC. PLoS Pathog 18(10): e1010805. https://doi.org/10.1371/journal.ppat.1010805
- A WHO-Strategic Research Agenda for Filovirus Research and Monitoring (WHO-AFIRM). https://www.who.int/publications/m/item/a-who-strategic-research-agenda-for-filovirus-research-and-monitoring—–(who-afirm)
- Building research readiness for a future filovirus outbreak, Workshop February 20 – 22, 2024, Uganda https://www.who.int/news-room/events/detail/2024/02/20/default-calendar/building-research-readiness-for-a-future-filovirus-outbreak-workshop-february-20-22-2024-uganda
- WHO Technical Advisory Group – candidate vaccine prioritization. Summary of the evaluations and recommendations on the four Marburg vaccines. https://www.who.int/publications/m/item/who-technical-advisory-group—candidate-vaccine-prioritization.–summary-of-the-evaluations-and-recommendations-on-the-four-marburg-vaccines
- Marburg virus vaccine landscape https://www.who.int/publications/m/item/marburg-virus-vaccine-landscape
- Marburgvirus therapeutics landscape https://www.who.int/publications/m/item/marburg-virus-therapeutics-landscape
- Considerations for border health and points of entry for filovirus disease outbreaks: https://www.who.int/publications/m/item/considerations-for-border-health-and-points-of-entry-for-filovirus-disease-outbreaks
Citable reference: World Health Organization (14 January 2024). Disease Outbreak News; Outbreak of suspected Marburg Virus Disease in the United Republic of Tanzania. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2025-DON552