Researchers at UT Southwestern Medical Center uncover key differences in fat infiltration within muscle and bone, paving the way for new treatments of age-related diseases.
A groundbreaking study led by researchers at UT Southwestern Medical Center has revealed significant sex-specific differences in how fat accumulates in muscle and bone, offering new insights into the development of musculoskeletal disorders and metabolic diseases. The findings, published in Diagnostics, could inform more targeted approaches to preventing and treating age-related conditions.
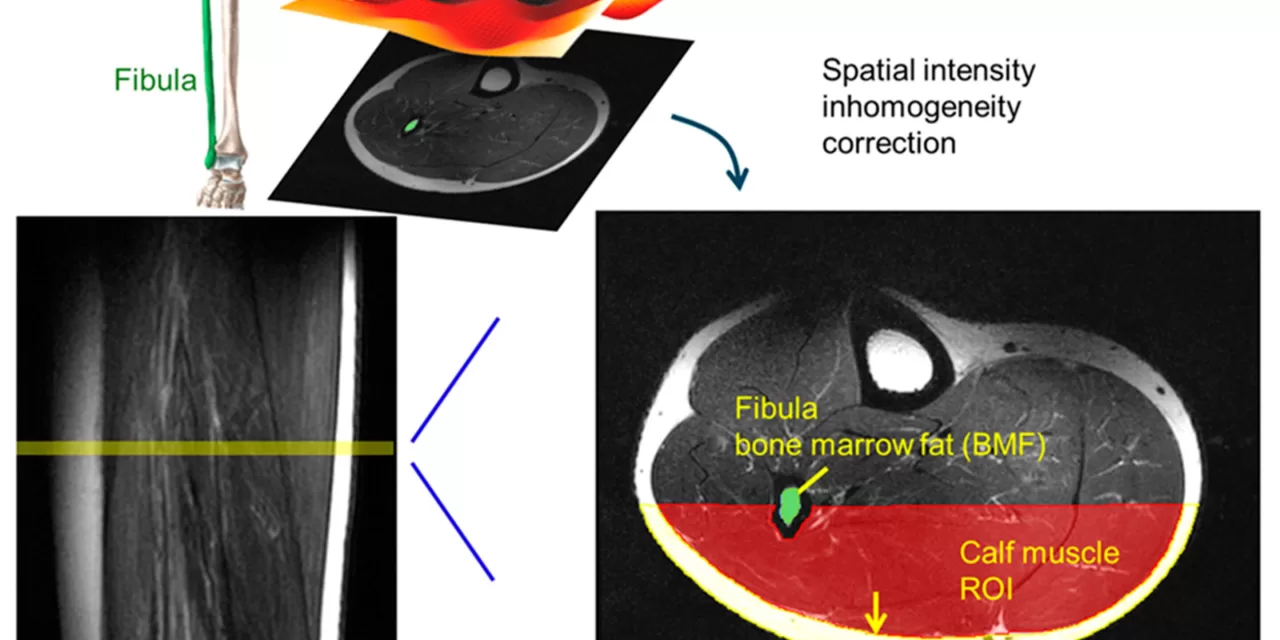
The research examined magnetic resonance imaging (MRI) scans of 107 patients, including 64 men and 43 women aged 11 to 79, representing diverse ethnicities and a wide range of body mass indices (BMI). The study focused on the lower extremities, uncovering critical patterns in fat infiltration within skeletal muscle (muscle fat infiltration, or MFI) and fat distribution in subcutaneous tissue and bone marrow. Researchers found distinct differences in how fat accumulates in these areas between men and women, shaped by both age and BMI.
“Musculoskeletal disorders are the leading cause of disability in the U.S., with enormous impacts on quality of life and longevity,” said Dr. Jimin Ren, the study’s senior author and an Associate Professor at UT Southwestern. “This study identifies key contributors to muscle fat infiltration, which can lead to muscle atrophy and dystrophy, two major factors in musculoskeletal dysfunction.”
One of the study’s major findings was that MFI increased significantly with age in women, while in men, MFI was more strongly correlated with body weight. Additionally, women exhibited almost double the average subcutaneous fat thickness compared to men (8.9 millimeters versus 4.3 millimeters), with this fat accumulation increasing with age in women, but decreasing in men, particularly in those who were not obese.
The researchers also observed a connection between MFI and bone marrow cross-sectional area (BMA), emphasizing the interdependence between muscle and skeletal health. Weakened bone structures may encourage fat infiltration into nearby muscles, which could lead to greater risks of falls, fractures, and metabolic disorders. These findings underscore the importance of maintaining overall musculoskeletal strength, especially in aging adults, to manage age-related health challenges.
Dr. Ren explained that skeletal muscle plays a vital role in regulating glucose metabolism, and when fat accumulates excessively within muscle, it can impair the muscle’s ability to process glucose. This, in turn, heightens the risk of insulin resistance and several associated conditions such as obesity, heart failure, stroke, sarcopenia, osteoporosis, chronic kidney disease, and Type 2 diabetes.
The study also highlights sex-specific health concerns related to aging. For instance, in women, hormonal changes post-menopause are likely to exacerbate the risks of sarcopenia (loss of muscle mass and strength) and osteoporosis (bone weakening). In men, the study found that fat infiltration was more strongly linked to body weight, emphasizing the importance of weight management to preserve muscle function.
The findings provide important insights into how sex, age, and BMI influence fat distribution in muscles and bones, offering a basis for the development of personalized interventions. These could include tailored exercise regimens, nutrition plans, and therapies aimed at preserving musculoskeletal health and preventing age-related decline.
Dr. Ren noted that the research holds promise for clinical care, particularly in terms of noninvasive screening and monitoring of muscle metabolic health. Markers such as subcutaneous fat thickness, intramuscular fat, and BMA could be used to assess the risk of sarcopenia and osteoporosis, leading to earlier interventions.
Lead author Dr. Talon Johnson, a postdoctoral research fellow in the Advanced Imaging Research Center (AIRC), explained, “By linking fat infiltration in muscle to fat in the bone marrow, our study suggests the possibility of dual-targeted therapies that support both muscle and bone health. This integrated approach could contribute to developing early interventions for the metabolic and musculoskeletal disorders that are becoming more common as we age.”
These new insights open up exciting opportunities for improving the treatment and prevention of musculoskeletal disorders, ultimately enhancing the quality of life for aging individuals.
For more information, refer to the study: Talon Johnson et al, Sex Differences in Fat Distribution and Muscle Fat Infiltration in the Lower Extremity: A Retrospective Diverse-Ethnicity 7T MRI Study in a Research Institute Setting in the USA, Diagnostics (2024). DOI: 10.3390/diagnostics14202260.