Philadelphia, PA – Researchers at the Children’s Hospital of Philadelphia (CHOP) and the University of Pennsylvania Perelman School of Medicine have unveiled a groundbreaking gene therapy model that could revolutionize treatment for X-linked sideroblastic anemia (XLSA). This rare and debilitating congenital anemia, caused by mutations in the ALAS2 gene, impairs the synthesis of heme—a vital component of hemoglobin—and leaves patients reliant on transfusions and supplements for survival.
The study, which represents the first exploration of gene therapy for XLSA, was published in the journal Blood and featured on its cover. It highlights the potential for this innovative treatment to address not only XLSA but also other disorders linked to heme synthesis.
Understanding XLSA and Its Challenges
XLSA predominantly affects males under 40, though recent cases among females and older individuals have surfaced. Symptoms include severe anemia, iron overload, extreme fatigue, shortness of breath, and growth delays. Current treatments involve lifelong reliance on pyridoxine (vitamin B6) supplements and blood transfusions. While allogenic stem cell transplants offer a potential cure, they are accessible to only a fraction of patients due to compatibility requirements, high costs, and the risks of intensive chemotherapy.
The Novel Gene Therapy Model
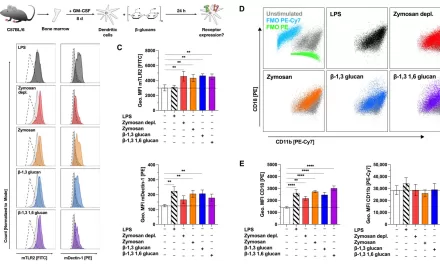
Led by Carlo Castruccio Castracani, PharmD, Ph.D., researchers employed a preclinical model to test a new approach. Using a targeted lipid nanoparticle (LNP) platform developed by co-senior author Hamideh Parhiz, PharmD, Ph.D., the team induced deletion of the ALAS2 gene in hematopoietic stem cells. This simulated XLSA in the model, manifesting hallmark symptoms like anemia, spleen enlargement, and ring sideroblasts—abnormal immature red blood cells.
“The absence of ALAS2 triggered an expansion of immature red cells, many of which died prematurely,” explained Castruccio Castracani. “We also observed significant mitochondrial dysfunction, which prevented the formation of healthy red cells and led to severe anemia.”
A Promising Lentiviral Gene Therapy
To counteract the effects of ALAS2 deficiency, the researchers developed a lentiviral vector to activate the human ALAS2 gene specifically in erythroid cells. This treatment restored hemoglobin production, improved red blood cell counts, and normalized iron metabolism in preclinical trials.
Subjects receiving the optimal dose of the vector demonstrated substantial improvements in anemia symptoms, spleen health, and iron balance. “This new model and vector could transform the lives of XLSA patients,” said Stefano Rivella, Ph.D., a senior author and pediatric hematology expert at CHOP.
Future Directions
The study’s success lays a foundation for further exploration of gene therapy and pharmacological interventions for XLSA and related diseases. Researchers aim to refine the model for in vivo gene editing and expand its application to other disorders of red blood cell production.
“This breakthrough underscores the power of targeted gene therapy to address diseases once considered incurable,” said Rivella.
For more information, refer to the study: An erythroid-specific lentiviral vector improves anemia and iron metabolism in a new model of XLSA (DOI: 10.1182/blood.2024025846).