December 30, 2024 – Mayo Clinic
Pancreatic cancer screening has seen significant progress in recent years, offering hope for earlier detection and improved survival rates. With new research-based guidelines and cutting-edge technologies like genetic testing and artificial intelligence (AI), healthcare professionals are better equipped to identify those at high risk and catch the disease in its early stages.
Who Should Be Screened for Pancreatic Cancer?
Screening is recommended for individuals at high risk, including those with a family history of pancreatic cancer or genetic mutations.
“The more relatives you have with pancreatic cancer, the greater your risk,” explains Dr. Michael Wallace, an interventional endoscopist at Mayo Clinic Comprehensive Cancer Center. Screening is generally advised for people with two first-degree relatives or three relatives of any degree affected by the disease.
Genetic testing is a vital tool for identifying risk, but uptake remains low. “Less than one-third of eligible individuals undergo genetic testing,” says Dr. Wallace, emphasizing its potential to save lives.
Additionally, a new diagnosis of diabetes accompanied by weight loss—particularly in individuals over 50—can be an early indicator of pancreatic cancer. Unlike the common form of diabetes linked to obesity, this type is associated with weight loss and warrants further evaluation, such as imaging or blood tests.
How Is Pancreatic Cancer Screening Conducted?
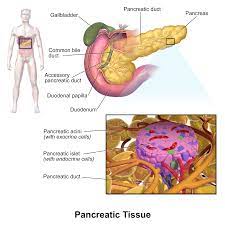
Two primary tests are recommended for pancreatic cancer screening:
- MRI – A non-invasive imaging method that provides detailed pictures of the pancreas.
- Endoscopic Ultrasound – A procedure that uses an endoscope equipped with an ultrasound device to obtain high-resolution images of the pancreas. If abnormalities are detected, the endoscope can also collect biopsies.
Dr. Wallace stresses the importance of undergoing these tests at specialized centers with experienced professionals. Screening is generally performed annually, often alternating between MRI and endoscopic ultrasound.
Advances in Pancreatic Cancer Screening
Genetic Testing and Screening Expansion
Efforts are underway to increase genetic testing awareness and usage. While genetic mutations account for only 10% of pancreatic cancer cases, identifying high-risk individuals enables early intervention.
For the remaining 90% of cases, researchers are exploring methods like analyzing pancreatic cyst fluid and pancreatic juices to assess cancer risk. Most pancreatic cysts are benign, but a small percentage can become malignant, making accurate screening essential.
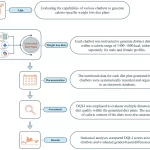
AI and Risk Classification
AI is playing an increasingly important role in identifying cancer risk. Dr. Wallace and his team are nearing the end of a five-year study evaluating an AI algorithm that classifies pancreatic cysts as high- or low-risk. Early results demonstrate the algorithm’s ability to analyze MRI scans in seconds, potentially improving accuracy and reducing the need for invasive procedures.
“These advances allow us to identify cysts likely to turn cancerous,” says Dr. Wallace. “We can intervene before cancer develops, improving outcomes.”
Future Directions in Screening
Researchers are also investigating the use of routine health metrics—such as body weight, blood sugar, and cholesterol levels—to predict pancreatic cancer risk. These indicators, already monitored during annual checkups, could help identify candidates for screening.
A Sense of Hope
Dr. Wallace emphasizes that advancements in genetic testing, AI, and screening technologies have already improved survival rates. Early detection remains key to shifting outcomes for pancreatic cancer patients.
“We’re making progress toward identifying risk and detecting cancer earlier,” says Dr. Wallace. “These innovations are giving us hope for a brighter future in pancreatic cancer care.”
This article is based on insights provided by Mayo Clinic.