Newcastle, UK — A groundbreaking lung scanning method developed by researchers at Newcastle University is transforming how lung diseases and transplants are monitored. By providing real-time imaging of lung function, this innovative approach could help medical professionals identify and address declines in lung performance sooner than ever before.
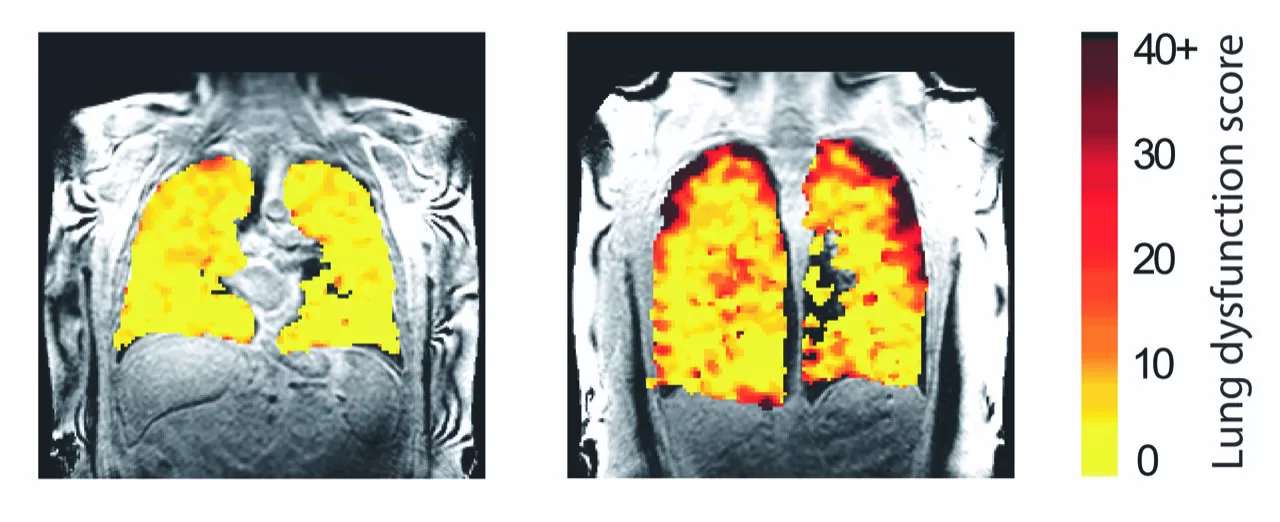
The technique utilizes a specialized gas, perfluoropropane, which is visible on MRI scans. Patients inhale the gas, allowing researchers to capture detailed images of airflow within the lungs. These scans reveal how effectively different parts of the lungs are ventilated and highlight regions with ventilation issues.
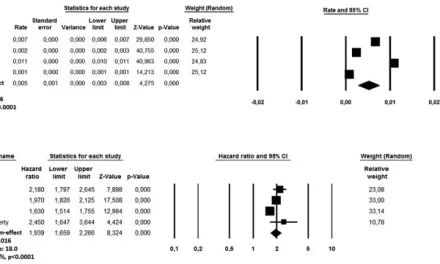
Led by Professor Pete Thelwall, Director of the Center for In Vivo Imaging at Newcastle University, the team tested the method on patients with asthma, chronic obstructive pulmonary disease (COPD), and lung transplant recipients. Their findings, published in Radiology and JHLT Open, underscore the potential of this technique in both clinical settings and medical research.
Real-Time Insights into Lung Function
The scans allow researchers to observe how air moves in and out of the lungs during each breath. For asthma and COPD patients, the team demonstrated that treatment effects could be quantified in real time. Using a commonly prescribed bronchodilator, salbutamol, researchers assessed improvements in lung ventilation, identifying which areas of the lungs responded to treatment.
“Our scans show where there is patchy ventilation in patients with lung disease and which parts improve with treatment,” explained Professor Thelwall. “For example, with asthma medication, we can see how specific lung regions become better ventilated.”
Advances in Lung Transplant Monitoring
In a complementary study, the team explored the use of the scanning method for lung transplant recipients. Chronic rejection, a common complication where the immune system attacks donor lungs, was detected with remarkable sensitivity.
Scans revealed that air movement was significantly impaired in patients experiencing chronic rejection, especially in the small airways. By identifying these changes earlier than conventional lung function tests, clinicians could intervene sooner to protect the transplanted lungs.
Professor Andrew Fisher, co-author and expert in respiratory transplant medicine, highlighted the potential impact of this work. “This new type of scan could allow us to detect early changes in lung function, enabling timely treatment to prevent further damage,” he said.
A Future of Improved Care
The sensitivity of this method makes it a promising tool for managing lung transplants and chronic respiratory conditions. By visualizing ventilation defects and quantifying treatment responses, the scans could revolutionize clinical trials and treatment strategies for lung diseases.
As the team continues to refine the technology, they are optimistic about its broader applications. “This innovation represents a significant step forward in how we monitor and treat lung diseases,” added Professor Thelwall.
References
- Pippard BJ et al., Radiology (2024). DOI: 10.1148/radiol.240949
- Mary A. Neal et al., JHLT Open (2024). DOI: 10.1016/j.jhlto.2024.100167