Researchers identify highly infectious and untreatable Klebsiella pneumoniae strains among war-wounded patients.
A groundbreaking study has revealed that pandrug-resistant bacteria isolated from war-wounded patients in Ukraine are not only impervious to all known antibiotics but also exceptionally aggressive and deadly. Published in the Journal of Infection, the research underscores the growing global health threat posed by antibiotic resistance, particularly in conflict zones where healthcare systems are under immense strain.
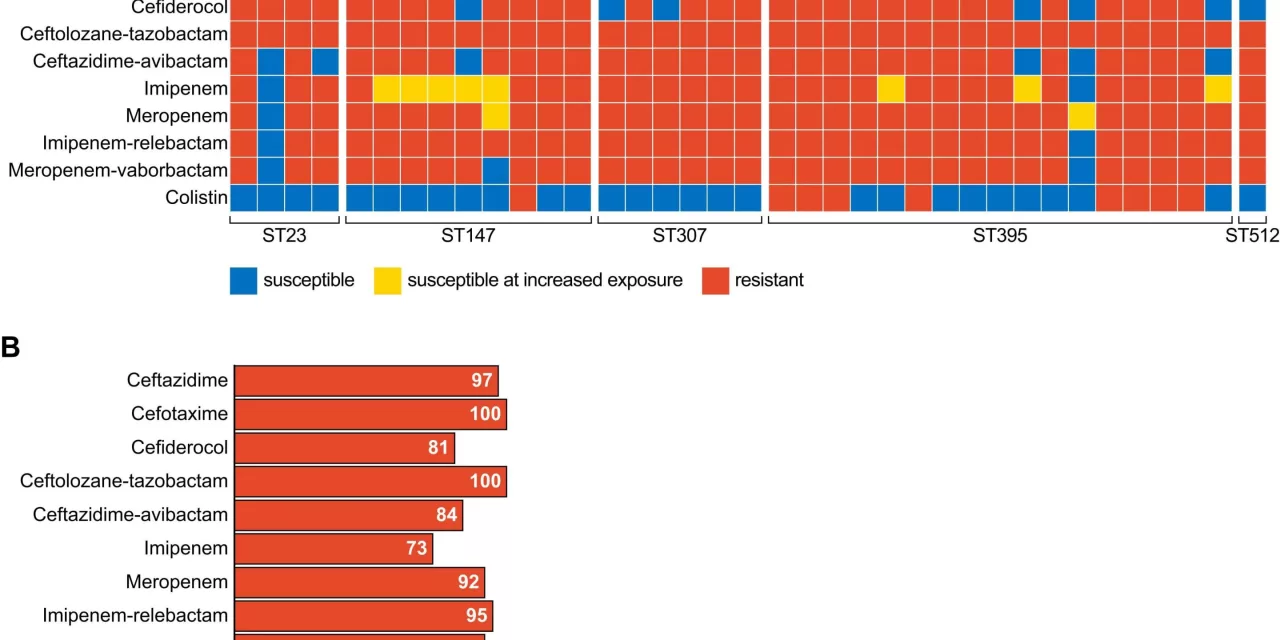
The study, led by Kristian Riesbeck, professor of clinical bacteriology at Lund University in Sweden, follows up on earlier findings that highlighted alarmingly high levels of antibiotic resistance among bacteria from war casualties. Using samples from 141 patients, including 133 war-wounded adults and eight newborns with pneumonia, researchers found that six percent of the bacteria were resistant to every antibiotic tested.
Among the most concerning findings was the bacterium Klebsiella pneumoniae, which has demonstrated not only complete resistance to antimicrobial drugs but also significant virulence. This bacterium is known to cause severe infections such as pneumonia, urinary tract infections, sepsis, and wound infections.
“Klebsiella pneumoniae with total resistance is both aggressive and dangerous,” Riesbeck explained. “Infections caused by these bacteria are very difficult, and in some cases impossible, to treat with existing medicines.”
A Dual Threat: Resistance and Virulence
Using genetic sequencing, the team confirmed that the resistant Klebsiella strains carried genes linked to both antibiotic resistance and enhanced pathogenicity. In experiments using mice and insect larvae, the most resistant strains were found to be the most lethal. The bacteria caused rapid deaths in insect larvae and survived more effectively in the lungs of mice infected with pneumonia.
“Typically, when bacteria become resistant, they lose some ability to cause disease because their energy is diverted to maintaining resistance. However, these strains from Ukraine are defying that trend, retaining both their resistance and their ability to cause severe infections,” Riesbeck noted.
Implications for Public Health
The findings highlight the compounding dangers of antibiotic-resistant infections in war zones. Ukraine’s ongoing conflict has severely disrupted healthcare infrastructure, creating conditions that facilitate the spread of resistant bacteria.
“This is a dire warning,” Riesbeck said. “The collapse of healthcare systems in war-torn areas, like Ukraine, exacerbates the spread of these deadly bacteria. Without proper isolation and treatment, these infections will persist and spread.”
The study’s results are a sobering reminder of the need for global action. Pandrug-resistant bacteria represent the most extreme form of antibiotic resistance and pose a growing challenge for healthcare systems worldwide.
A Global Wake-Up Call
Riesbeck called for heightened vigilance and investment in both antibiotic research and strategies to prevent the spread of resistant bacteria in conflict zones. He emphasized that the lessons from Ukraine are relevant to other regions experiencing war and healthcare crises.
“Even as these bacteria fight to survive antibiotic treatments, they retain their ability to cause severe disease,” Riesbeck said. “This is a frightening development and a warning for the future.”
As wars and healthcare collapses persist globally, the specter of untreatable infections looms large. The study underscores the urgent need for international cooperation to address the mounting threat of antibiotic-resistant pathogens.
For more information, refer to the original research: Oskar Ljungquist et al., “Pandrug-resistant Klebsiella pneumoniae isolated from Ukrainian war victims are hypervirulent,” published in the Journal of Infection (2024).