November 12, 2024
A new clinical practice report published in the New England Journal of Medicine (NEJM) calls for less invasive medical therapies as the first-line treatment for uterine fibroids, suggesting they are a safer and more effective alternative to hysterectomy, which remains the most common procedure for fibroid treatment. This report, written by Dr. Elizabeth A. Stewart and Dr. Shannon K. Laughlin-Tommaso from the Mayo Clinic, aims to raise awareness of newer, uterus-sparing treatments among gynecologists and primary care physicians.
The authors advocate for early diagnosis and treatment of fibroids, using hormone therapy, uterine-artery embolization, focused ultrasound ablation, and radiofrequency ablation as primary management tools. “This is not a new guidance but an invited clinical practice paper,” Dr. Laughlin-Tommaso explained, emphasizing the need for greater awareness around non-surgical treatments that could reduce recovery time and provide faster symptom relief.
Why Shift Away from Hysterectomy?
Hysterectomy is often favored for its definitive outcome—complete removal of fibroids and elimination of symptoms. However, it has long-term health impacts, including increased risk of cardiovascular issues, dementia, and reduced quality of life. Research also suggests that preserving the uterus and ovaries can have health benefits. Yet, studies show that nearly 60% of women undergoing hysterectomy for fibroids had no prior conservative treatments, which reflects the lack of widespread adoption of less invasive options.
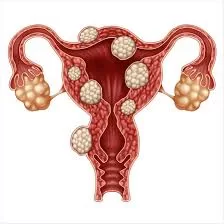
Dr. Laughlin-Tommaso points out that fibroids are particularly prevalent among Black women, affecting up to 80% of women with a uterus, with symptoms ranging from heavy menstrual bleeding to pelvic pressure and pain. Symptom relief is crucial, but treatments that preserve the uterus should be prioritized, especially for women who wish to retain fertility.
New Treatment Options and Recommendations
The NEJM report highlights several treatment options beyond hysterectomy, including:
- Medical therapies: Hormonal treatments such as contraceptives can manage bleeding, while newer options like oral GnRH antagonists offer more effective symptom relief with fewer side effects, such as hot flashes and nausea.
- Uterine-Artery Embolization: This minimally invasive procedure cuts blood supply to fibroids, causing them to shrink and reducing symptoms.
- Focused Ultrasound and Radiofrequency Ablation: These methods target individual fibroids with energy to reduce their size, providing symptom relief without removing the uterus.
- Myomectomy: Surgical removal of fibroids, often chosen by patients wishing to conceive, is also discussed. However, it has a high recurrence rate, with new fibroids developing in up to 50% of cases within five years.
Implications for Primary Care and Gynecology
This clinical review highlights a gap in fibroid care, particularly among general practitioners who may not be as familiar with the latest treatments. According to Dr. Sandra Hurtado, an OB/GYN at UTHealth in Houston, the report’s diagrams will be a valuable tool for non-specialists, helping them better explain treatment options to patients.
Dr. Charles J. Ascher-Walsh of Mount Sinai, who was not involved in the study, praised the report’s accessibility in NEJM and its potential to increase awareness and funding for research in this underfunded field.
Next Steps in Fibroid Care
The report emphasizes the need for more research and early screening. Additionally, it suggests developing risk-prediction models and staging systems to better manage fibroid treatment. For primary care physicians, early diagnosis and conservative treatments could reduce the number of unnecessary hysterectomies.
In a case study included in the report, a 33-year-old Black woman with heavy bleeding and anemia was treated with oral GnRH therapy, highlighting the paper’s emphasis on preserving fertility and managing fibroid symptoms without surgery.
The authors call for more funding to address disparities in fibroid treatment, especially among Black and Latina women, citing connections to vitamin D deficiency, stress, and socioeconomic factors as possible contributors to the higher prevalence in these groups.
This clinical practice summary, while not introducing new guidelines, aims to educate a wider audience on the benefits of uterus-sparing treatments, advocating a patient-centered approach that values long-term health outcomes and quality of life over the immediacy of surgery.